New screening modalities and the customization of the screening population could soon change the way that screening for colorectal cancer is done. At Digestive Disease Week 2014, the largest gathering of gastrointestinal disease specialists in the world, researchers presented data suggesting that at least some of these changes are just around the bend.
Stool DNA vs Fecal Immunochemical Testing
There was much buzz about the noninvasive multitarget stool DNA testing (Cologuard), which was recently recommended by the U.S. Food and Drug Administration (FDA)’s Molecular and Clinical Genetics advisory committee. The new test involves quantitative molecular assays for KRAS mutations, aberrant NDRG4 and BMP3 methylation, and beta-actin, plus a hemoglobin immunoassay.
Co-investigator for the studies, David A. Ahlquist, MD, the Carol Gatton Professor of Gastrointestinal Research at the Mayo Clinic, Rochester, said that should multitarget stool DNA testing become FDA-approved, many may choose to use this test because of its user-friendly features and high early-detection accuracy.
“We are hoping the stool DNA test will become a legitimate part of our armamentarium,” he said in a panel discussion at Digestive Disease Week. Compared with colonoscopy, the test is noninvasive but would be performed more often—probably every 3 years—with referral to colonoscopy for patients with positive findings. “Fine-tuning of this algorithm will require additional observation,” he added.
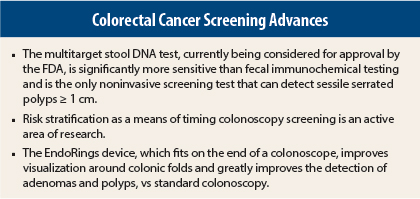
Data from the DEEP-C trial of nearly 10,000 individuals suggests multitarget stool DNA testing is more effective than currently available fecal immunochemical testing in detecting adenocarcinoma (92.3% vs 73.8%; P = .002), advanced precancerous lesions (42.4% vs 23.8%; P < .001), polyps with high-grade dysplasia (69.2% vs 46.2%; P = .004) and serrated sessile polyps measuring ≥ 1 cm (42.4% vs 5.1%; P = .001), though fecal immunochemical testing is more specific (94.9%–96.4% vs 86.6%–89.8%). These results were recently published in The New England Journal of Medicine.1
At Digestive Disease Week, the DEEP-C investigators presented the prespecified analysis for sessile serrated polyps ≥ 1 cm. These lesions are frequent precursors to cancer and are often missed by colonoscopy as well as by fecal immunochemical testing, since they do not bleed. For detecting these challenging lesions, multitarget stool DNA testing was almost 10 times better than fecal immunochemical testing, the study found.2
Of the whole study population, 7.6% had an advanced precancerous lesion as the most advanced finding on colonoscopy and 13.1% of these individuals had a sessile serrated polyp ≥ 1 cm, for an overall incidence in the population of 1%.
“The detection of patients with [sessile serrated polyps] is a clinically important issue in the consideration of noninvasive screening techniques. The sensitivity of [multitarget stool DNA testing] for [sessile serrated polyps] ≥ 1 cm was significantly higher than that of fecal immunochemical testing, which was not effective for identifying patients with large [sessile serrated polyps],” said Barry M. Berger, MD, Chief Medical Officer of EXACT Sciences, Madison, Wisconsin, who presented the subset analysis.
“Stool DNA testing really is the only noninvasive approach to detecting these lesions,” Dr. Ahlquist agreed.
Integration Into Screening Algorithm
The detection of 92% of colon cancer is considered extremely high for a noninvasive test and spares these patients colonoscopy, expert endoscopists commented. One of these was Douglas Rex, MD, Professor of Medicine at the University of Indiana, Indianapolis, who often speaks about the potential “disruption” of colonoscopy as the preferred screening approach.
Dr. Rex called the sensitivity “remarkable for a noninvasive test,” but he indicated that the test might be expensive (the price has not yet been set). While this may not be a factor for individuals who can pay for it, it could be problematic in terms of its widespread uptake and for the health-care system at large, he maintained.
“I don’t think colonoscopy is off the map as a screening option. We are wrestling with several legitimate strategies right now,” he said in a panel discussion.
Thomas F. Imperiale, MD, Professor of Medicine at Indiana University School of Medicine, Indianapolis, who authored the pivotal study, added, “How this new test integrates into the current options for colorectal cancer screening will depend on its comparative effectiveness and cost-effectiveness—metrics that may be best delineated through the use of microsimulation modeling. Based on test characteristics alone, [multitarget stool DNA testing] may be best for persons between 50 and 64 years old for whom the prevalence of disease is lower and test specificity is higher, characteristics that minimize the false-positive risk and optimize the positive-predictive value of the test.”
Risk Stratification for Screening
Screening colonoscopy may not always be a “one size fits all” situation, according to a number of specialists who suggest that risk stratification makes sense. Several adverse risk factors have been established, but only age (50 as the threshold) and family history (one or more first-degree relatives with colorectal cancer or adenoma) are used in clinical decision-making. This leaves out black race, male sex, cigarette smoking, high body mass index, heavy ethanol use, diet (red meat), and diabetes.
Dr. Imperiale pointed out that while colorectal cancer screening of average-risk individuals reduces colorectal cancer–related morbidity and mortality, it is inefficient and expensive. More than half the population is never screened, many low-risk persons are screened unnecessarily, and many high-risk persons are never examined.
A tailored colorectal cancer screening design would adjust the intensity of screening to the individual’s risk and optimize the balance between benefit and risk. Screening would be more aggressive for high-risk groups, and could be delayed or performed with noninvasive tests in low-risk persons, said Dr. Imperiale.
Dr. Imperiale and his colleagues, therefore, constructed a risk-based model using literature-derived risk factors and correlated the scores with endoscopic and pathologic findings among 4,500 individuals.3 With the application of the model, they were able to stratify risk for three-fourths of an average-risk cohort, resulting in a high-risk group in which colonoscopy had a high yield for advanced neoplasia, and a low-risk group that could be screened less invasively.
“If validated in independent cohorts, this strategy could improve the efficiency and uptake of [colorectal cancer] screening,” Dr. Imperiale said.
Could individuals simply be stratified by age and race? Age-adjusted colorectal cancer risk is higher in men than in women—a 10-year lag in cancer risk is observed in women, with the exception of black women, whose risk is comparable to that of men the same age. Black individuals have higher colorectal cancer incidence and mortality, possibly because of an earlier onset of cancer precursors, more aggressive tumor biology, or less access or adherence to screening. Therefore, they may warrant earlier or more intensive screening, experts have suggested.
David Lieberman, MD, Head of Gastroenterology at Oregon Health & Science University, Portland, who has conducted much of the research in this area, said risk-based screening is rational. However, he worries that it would only complicate efforts at colorectal cancer prevention.
“We showed in a screening cohort that a few simple things—age, sex, race/ethnicity—were strongly associated with the risk of advanced neoplasia,” he said. “But in discussing the guidelines for screening, our sense was that we are already delivering a complicated message by offering a menu of screening options, and that by further complicating it—stratifying by risk—we might paradoxically adversely affect screening rates,” he continued.
“We have been making progress, and we don’t want to complicate things, but I am suggesting that now, perhaps, the clouds have opened, and it’s time to start thinking about a more customized approach,” he said in a panel discussion.
New Colonoscopy Technology
The addition of a small rubber tip with flexible, circular rings to the distal end of a colonoscope resulted in substantially greater detection of polyps and adenomas in a randomized, tandem study of 106 patients evaluating the EndoRings device.4
In a per-lesion analysis, the adenoma miss rate was 13% when patients underwent an EndoRings colonoscopy followed by a standard colonoscopy and 53% when standard colonoscopy was done before the EndoRings colonoscopy (P > .001). Similarly, the miss rates for polyps were 11% and 58% (P > .001), investigators of the Dutch CLEVER study reported.
This is a big improvement over the current adenoma miss rate of 25% to 40% with standard colonoscopy techniques. Lack of detection is largely due to inadequate visualization of proximal aspects of folds and inner curves of flexures, which can be overcome by the EndoRings device, which improves visualization by engaging and stretching colonic folds during withdrawal, explained Peter D. Siersema, MD, PhD, Director of Gastroenterology and Hepatology at University Medical Center Utrecht, the Netherlands. The EndoRings device will soon be available in the United States and Europe. ■
Disclosure: Dr. Ahlquist, as co-developer of the multitarget stool DNA test, will receive inventor’s share of royalties coming to the Mayo Clinic from Exact Sciences; he is also a scientific advisor to an research collaborator with Exact Sciences. Dr. Berger is an employee of Exact Sciences Corporation. Dr. Rex reported consulting and board membership with Exact Sciences Corporation. Dr. Siersema reported grant/research support from EndoAid Ltd. Dr. Imperiale had no relevant disclosures.
References
1. Imperiale TF, Ransohoff DF, Itzkowitz SH, et al: Multi-target stool DNA testing for colorectal-cancer screening. N Engl J Med 370:1287-1297, 2014.
2. Berger BM, Imperiale TF, Hilsden RJ, et al: Non-invasive detection of sessile serrated polyps in an average risk colorectal cancer screening population: Comparison of multi-target stool DNA and fecal immunochemical testing. Digestive Disease Week 2014. Abstract 113. Presented May 3, 2014.
3. Imperiale TF, Monahan PO, Stump TE, et al: A risk stratification strategy for colorectal cancer screening: sequential application of two clinical prediction rules. Digestive Disease Week 2014. Abstract 225. Presented May 3, 2014.
4. Dik VC, Grainek IM, Segol O, et al: Comparing standard colonoscopy with EndoRings colonoscopy: A randomized, multicenter tandem colonoscopy study—interim results of the CLEVER study. Digestive Disease Week 2014. Abstract 929b. Presented May 6, 2014.