Approximately 15% of patients with breast cancer have tumors that overexpress the HER2 protein and these patients can benefit from HER2-targeted therapies. The American Society of Clinical Oncology recently released a clinical practice guideline on systemic therapy for patients with advanced HER2-positive breast cancer, published in the Journal of Clinical Oncology.1 The rationale for the guideline is that several new agents have become available for treatment of metastatic HER2-positive breast cancer since the approval of trastuzumab (Herceptin).
Up to half of all patients with HER2-positive metastatic breast cancer develop brain metastases over time. Recommendations for the management of brain metastases in patients with HER2-positive breast cancer are detailed in another recently released companion guideline.2
The guideline recommendations were developed by a multidisciplinary group of experts based on a systematic review of phase III randomized controlled trials and clinical experience. Literature searches identified a total of 16 eligible randomized controlled trials reported between 2009 and 2012, consisting of 9 first-line, 3 second-line, and 4 post–second-line trials. Three first-line hormonal therapy plus HER2-targeted therapy trials addressed the role of hormonal/endocrine therapy, and two trials addressed the issue of how prior adjuvant HER2-targeted therapy might influence subsequent treatment choices. Outcomes of interest included overall survival, progression-free survival, and adverse events.
The ASCO expert panel was co-chaired by Sharon H. Giordano, MD, of The University of Texas MD Anderson Cancer Center, Houston, and Eric P. Winer, MD, of Dana-Farber Cancer Institute, Boston.
Primary Clinical Question
The primary clinical question addressed by the guideline is: “What is the optimal medical therapy for advanced HER2–positive breast cancer, specifically HER2-targeted therapy, either alone or in combination with chemotherapy and/or endocrine therapy?” The guideline recommendations are summarized below, along with notation of type of recommendation, evidence quality, and strength of recommendation.
General Recommendations
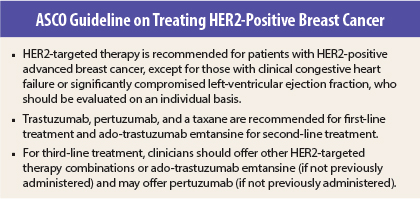
According to the guideline, clinicians should recommend HER2-targeted therapy–based combinations for first-line treatment, except in highly selected patients with estrogen receptor–positive or progesterone receptor–positive and HER2-positive disease; in such patients, endocrine therapy alone may be used. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
For patients with disease progressing during or after first-line HER2-targeted therapy, clinicians should recommend second-line HER2-targeted therapy-based treatment. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
For patients with disease progressing during or after second-line or greater HER2-targeted treatment, clinicians should recommend third-line or greater HER2-targeted therapy-based treatment. (Type = evidence based, evidence quality = intermediate, strength of recommendation = moderate.)
Specific Regimens
Clinicians should recommend the combination of trastuzumab, pertuzumab (Perjeta), and a taxane for first-line treatment, unless the patient has a contraindication to taxanes. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
For patients with disease progressing during or after first-line HER2-targeted therapy, clinicians should recommend ado-trastuzumab emtansine (Kadcyla) as second-line treatment. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
For patients with disease progressing during or after second-line or greater HER2-targeted therapy who have not received ado-trastuzumab emtansine, clinicians should offer ado-trastuzumab emtansine. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
For patients with disease progressing during or after second-line or greater HER2-targeted treatment who have not received pertuzumab, clinicians may offer pertuzumab. (Type = informal consensus, evidence quality = insufficient, strength of recommendation = weak.)
For patients with disease progressing during or after second-line or greater HER2-targeted treatment who have already received pertuzumab and ado-trastuzumab emtansine, clinicians should recommend third-line or greater HER2-targeted therapy- based treatment. Options include lapatinib (Tykerb) plus capecitabine, as well as other combinations of chemotherapy and trastuzumab, lapatinib and trastuzumab, or hormonal therapy (in patients with estrogen receptor–positive and/or progesterone receptor–positive disease). There is insufficient evidence to recommend one regimen over another. (Type = informal consensus, evidence quality = insufficient, strength of recommendation = weak.)
Chemotherapy Duration
In patients receiving HER2-targeted therapy and chemotherapy combinations, chemotherapy should continue for approximately 4 to 6 months (or longer) and/or to the time of maximal response, depending on toxicity and in the absence of progression. When chemotherapy is stopped, clinicians should continue HER2-targeted therapy; no further change in the regimen is needed until the time of progression or unacceptable toxicities. (Type = evidence based, evidence quality = intermediate, strength of recommendation = moderate.)
Patients Who Received Adjuvant Trastuzumab
For patients finishing trastuzumab-based adjuvant treatment ≤ 12 months before recurrence, clinicians should follow the second-line HER2-targeted therapy- based treatment recommendations. (Type = evidence based, evidence quality = intermediate, strength of recommendation = moderate.)
For patients finishing trastuzumab-based adjuvant treatment > 12 months before recurrence, clinicians should follow the first-line HER2-targeted therapy–based treatment recommendations. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
Endocrine Therapy
For patients with hormone receptor–positive and HER2-positive disease, clinicians may recommend:
- HER2-targeted therapy plus chemotherapy. (Type = evidence based, evidence quality = high, strength of recommendation = strong.)
- Endocrine therapy plus trastuzumab or lapatinib (in selected cases). (Type = evidence based, evidence quality = high, strength of recommendation = moderate.)
- Endocrine therapy alone (in selected cases). (Type = evidence based, evidence quality = intermediate, strength of recommendation = weak.)
For patients who have started with a HER2-positive targeted therapy and chemotherapy combination, clinicians may add endocrine therapy to the HER2-targeted therapy when chemotherapy ends and/or when the cancer progresses. (Type = informal consensus, evidence quality = insufficient, strength of recommendation = weak.)
In special circumstances, such as low disease burden, presence of comorbidities (contradictions to HER2-targeted therapy such as congestive heart failure), and/or presence of a long disease-free interval, clinicians may offer first-line endocrine therapy alone. (Type = informal consensus, evidence quality = intermediate, strength of recommendation = weak.)
Qualifying statement: Although clinicians may discuss using endocrine therapy with or without HER2-targeted therapy, the majority of patients will still receive chemotherapy plus HER2-targeted therapy. ■
Disclosure: For full disclosures of the guideline authors, visit jco.ascopubs.org.
References
1. Giordano SH, Temin S, Kirshner JJ, et al: Systemic therapy for patients with advanced human epidermal growth factor receptor 2–positive breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. May 5, 2014 (early release online).
2. Ramakrishna N, Temin S, Chandarlapaty S, et al: Recommendations on disease management for patients with advanced human epidermal growth factor receptor 2–positive breast cancer and brain metastases: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. May 5, 2014 (early release online).