Patients with breast cancer and deficient levels of 25-hydroxy-vitamin D are more likely to have aggressive tumor profiles and unfavorable prognostic markers than women with optimal levels of vitamin D, according to research presented at the 12th Annual Meeting of the American Society of Breast Surgeons, held in Washington, DC.1
 “This is one of only a few studies to examine the role of vitamin D in breast cancer progression, rather than in cancer development. The magnitude of the findings was quite surprising,” said Luke J. Peppone, PhD, Research Assistant Professor of Radiation Oncology at the University of Rochester Medical Center, Rochester, New York, a study investigator.
“This is one of only a few studies to examine the role of vitamin D in breast cancer progression, rather than in cancer development. The magnitude of the findings was quite surprising,” said Luke J. Peppone, PhD, Research Assistant Professor of Radiation Oncology at the University of Rochester Medical Center, Rochester, New York, a study investigator.
Mounting data point to a role for vitamin D deficiency in the development of breast cancer. The current study linked vitamin D deficiency with prognostic factors and outcomes.
“Vitamin D deficiency is common among patients with breast cancer. The vitamin D receptor modulates cell-cycle proliferation, induction of differentiation, and activation of apoptosis,” co-investigator Kristin Skinner, MD, also of the University of Rochester, explained in a press briefing.
The study examined the association between vitamin D levels around the time of diagnosis with demographic, pathologic, and genetic characteristics of breast cancer in 194 patients at the University of Rochester Medical Center. Noncancer controls were selected from among the 37,337 women who underwent vitamin D testing at the University during the same time period.
Vitamin D levels were classified as optimal (≥ 32 ng/mL), suboptimal (< 32 ng/mL), insufficient (20–31 ng/mL), or deficient (< 20 ng/mL).
Notable Associations
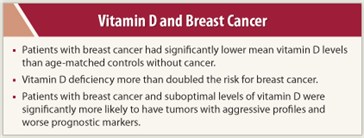
 “Our patients with breast cancer had significantly lower mean vitamin D levels than age-matched noncancer controls,” Dr. Skinner announced. “If you were deficient, the odds ratio for developing breast cancer was 2.4, compared to a woman with optimal levels.”
“Our patients with breast cancer had significantly lower mean vitamin D levels than age-matched noncancer controls,” Dr. Skinner announced. “If you were deficient, the odds ratio for developing breast cancer was 2.4, compared to a woman with optimal levels.”
A woman with breast cancer was 1.76 times more likely to be deficient in vitamin D, vs controls, she added.
Mean 25-hydroxy-vitamin D level was 37.4 ng/mL in controls, compared with 32.7 ng/mL in patients with breast cancer (P = .002).
Patients with breast cancer and suboptimal levels of vitamin D were also more likely to have tumors with more aggressive profiles and worse prognostic markers, such as estrogen receptor (ER)-negative status, triple-negative tumors, basal-like molecular phenotype, and Oncotype DX high-risk tumors, the study found.
 The odds ratios for some of the most notable associations were:
The odds ratios for some of the most notable associations were:
- non-Caucasian race: 3.6
- basal-like gene profile (vs luminal A/B): 3.4
- Oncotype recurrence score > 18 (vs ≤ 18): 3.2
- triple-negative breast cancer: 3.1
- ER-negative status: 2.6
- premenopausal status: 2.3
- invasive breast tumors: 2.2
Older women had significantly higher mean vitamin D levels than younger women, she added.
“These results may help to explain the observed decreased survival rate among vitamin D–deficient patients with breast cancer and the poorer prognosis seen in young, premenopausal, and non-Caucasian patients,” Dr. Skinner suggested.
Dr. Skinner routinely measures vitamin D in her patients and prescribes replacement treatment (1,000–2,000 IU/d) if they are low. “We get them above 32 ng/mL, then we titrate replacement to reach 50 ng/mL,” she told The ASCO Post. ■
Financial Disclosure: Dr. Peppone and Dr. Skinner reported no potential conflicts of interest.
Reference
1. Rickles A, Peppone L, Huston A et al: Serum 25-hydroxyvitamin D and prognostic tumor characteristics in breast cancer patients. American Society of Breast Surgeons 12th Annual Meeting. Abstract 1701. Presented April 29, 2011.

 Julie R. Gralow, MD, Professor of Oncology at the University of Washington, Seattle, said the data reported by Rickles et al at the American Society of Breast Surgeons Annual Meeting support the Goodwin study presented at the 2008 ASCO Annual Meeeting.1 In that earlier Canadian cohort of 512 women, ...
Julie R. Gralow, MD, Professor of Oncology at the University of Washington, Seattle, said the data reported by Rickles et al at the American Society of Breast Surgeons Annual Meeting support the Goodwin study presented at the 2008 ASCO Annual Meeeting.1 In that earlier Canadian cohort of 512 women, ...