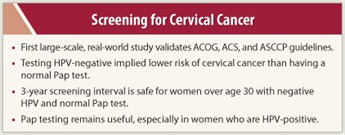
A large, “real-world” study has validated current recommendations from the American Congress of Obstetricians and Gynecologists (ACOG), American Cancer Society (ACS), and American Society for Colposcopy and Cervical Pathology (ASCCP) endorsing a 3-year cervical cancer screening interval for women over age 30 with a negative human papillomavirus (HPV) test and a normal Pap test. Furthermore, testing HPV-negative resulted in a very low risk of cancer that was not appreciably reduced by also having a normal Pap test. However, Pap testing remained important for HPV-positive women, because an abnormal Pap test helped identify even more women who developed cancer or precancer. The study was highlighted at a pre–Annual Meeting ASCO press briefing.
Large-scale Study
 “This first large-scale study of concurrent HPV and Pap testing for cervical cancer in routine clinical practice in the United States found that women who tested HPV-negative had an extremely low risk of cervical cancer. This finding demonstrates that a 3-year screening interval is safe,” said Hormuzd Katki, PhD, lead investigator, Division of Cancer Epidemiology and Genetics at NCI.
“This first large-scale study of concurrent HPV and Pap testing for cervical cancer in routine clinical practice in the United States found that women who tested HPV-negative had an extremely low risk of cervical cancer. This finding demonstrates that a 3-year screening interval is safe,” said Hormuzd Katki, PhD, lead investigator, Division of Cancer Epidemiology and Genetics at NCI.
Although the Pap test is an effective screening method for cervical cancer, 11,000 new cases develop annually in the United States, and cervical cancer accounts for 4,000 deaths each year. HPV causes almost every cervical cancer, but there is typically a 20-year interval between infection with HPV and the development of cervical cancer. Based on several clinical trials and research cohorts showing that HPV testing could further reduce cancer rates when done in concert with the Pap test, guidelines from ACOG, ACS, and ASCCP incorporated concurrent HPV testing with Pap testing at each clinical visit for women over age 30 (ie, co-testing). Guidelines currently recommend a 3-year interval for women who are HPV-negative and have a normal Pap smear.
Despite the existence of these guidelines, co-testing has not been widely adopted by physicians and by women, who may fear that extending the screening interval beyond 1 year is not safe, Dr. Katki explained. “The last piece of evidence required is to show that the 3-year screening interval is safe in routine clinical practice,” he noted.
Study Specifics
 The NCI-initiated study was done in collaboration with Kaiser Permanente Northern California to test the safety of the current ACOG, ACS, and ASCCP guidelines in a real-world patient population. The study included 331,818 women age 30 and older enrolled in the Kaiser Permanente Northern California’s co-testing program between 2003 and 2005. The women were followed through 2009.
The NCI-initiated study was done in collaboration with Kaiser Permanente Northern California to test the safety of the current ACOG, ACS, and ASCCP guidelines in a real-world patient population. The study included 331,818 women age 30 and older enrolled in the Kaiser Permanente Northern California’s co-testing program between 2003 and 2005. The women were followed through 2009.
Testing HPV-negative implied lower risk of cervical cancer than having a normal Pap test. The 5-year risk of cancer for women who were HPV-negative and had a normal Pap test was only 3.2 per 100,000 women per year. Looking at each test separately, a negative HPV test was associated with a 5-year risk of 3.8 cervical cancers per 100,000 women per year; a normal Pap test was associated with a 5-year risk of 7.5 cervical cancers per 100,000 women per year.
The HPV test identified more women at high risk of cancer or precancer than the Pap test. Women who were HPV-positive had a 7.6% 5-year risk of cervical cancer or precancer, whereas women with an abnormal Pap test had only a 4.7% 5-year risk of cervical cancer or precancer. In contrast, women testing HPV-negative had a 0.2% 5-year risk of cervical cancer or precancer, while women with a normal Pap test had a 0.4% 5-year risk of cervical cancer. “These findings demonstrate the superior ability of HPV testing to separate women into groups at high and low risk of cancer and precancer,” Dr. Katki stated.
Pap Testing Remains Useful
However, Dr. Katki emphasized that the Pap test remained useful for HPV-positive women. “For HPV-positive women, a positive Pap test identified an additional 6 in 100 women at risk for cervical cancer or precancer over 5 years,” he noted. “For HPV-positive women, abnormal Pap tests help identify immediate disease, whereas a normal Pap test signifies that cancer, if it occurs, is more likely to develop in the future.”
Based on their findings, the authors suggest that a screening program with a single HPV test could be used first, and if negative, no additional testing would be needed for at least 3 years; the Pap test would be reserved only for women who were HPV-positive. “This program could retain nearly all the safety of co-testing, but in our population, would have reduced the number of Pap tests by 95%. Still, we need to test this hypothesis in practice,” Dr. Katki stated. He pointed out that if the HPV test is positive, the same sample could be used for the Pap test, avoiding a second visit for the Pap test. ■
Financial Disclosure: Dr. Katki reported no potential conflicts of interest.
Reference
1. Katki HA, Kinney WK, Fetterman B, et al: Cervical cancer risk for 330,000 women undergoing concurrent HPV testing and cervical cytology in routine clinical practice. J Clin Oncol 29(15 suppl):Abstract 1508, 2011.

 This is a wonderful population-based study… that makes us comfortable with the current recommendations. The issue of how frequently one or the other test should be used is an evolving area,” said George W. Sledge, Jr, MD. Dr. Sledge is ASCO Immediate Past President.
This is a wonderful population-based study… that makes us comfortable with the current recommendations. The issue of how frequently one or the other test should be used is an evolving area,” said George W. Sledge, Jr, MD. Dr. Sledge is ASCO Immediate Past President.