The Immune-Related Adverse Events (irAE) Consortium has launched ASPIRE and STORIES with the aim of uniting clinicians, researchers, and patients to advance clinical care and advocacy. As the indications for immune checkpoint inhibitors in oncology have rapidly expanded over the past decade, the recognition and management of immune-related adverse events have experienced a rapid parallel evolution. Both the dissemination of current best practices and improvement of therapies for the broad spectrum of these autoinflammatory conditions remain challenging. With the increasing use of immune checkpoint inhibitors in earlier stages of disease and continued development of novel combination strategies, immune-related adverse events have become more common in oncologic practice. These events can affect multiple organ systems simultaneously or sequentially, demonstrating a capacity for unexpected and serious presentations.

Kriti Mittal, MD, MS

Kerry L. Reynolds, MD

Pauline Funchain, MD
As a new spectrum of de novo iatrogenic autoimmune conditions, the emergence of immune-related adverse events has necessitated a dedicated focus on clinical care, medical research, and therapeutic advancement. As a discipline, immune-related adverse events management exemplifies the growing logistical challenge of the essential but overloaded multidisciplinary model in oncology, in both outpatient and inpatient settings. There is an urgent need to empower clinicians, patients, and caregivers to create care models that are effective across various care settings in our health-care system.
Think Tank Collaboration
The irAE Consortium was created to tackle these challenges and unite like-minded and interested individuals. The inaugural meeting of the Consortium on March 7, 2024, held at Cleveland Clinic, found representatives from 28 organizations—academic, nonprofit, and industry partners—collaborating in a think tank aimed at advancing an agenda specific to immune-related adverse events, to improve patient care and promote scientific progress. During this first meeting, stakeholders developed a shared framework for a scientific consortium and a patient advocacy group, establishing the Alliance for Support and Prevention of Immune-Related Events (ASPIRE) and Standing Together to Optimize Research, Interventions, and Educations in irAEs (STORIES) as sister organizations.
In addition to the invested faculty at the numerous represented institutions, cofounding members of this initiative included Project Data Sphere, a nonprofit initiative of the CEO Roundtable on Cancer that leverages pooled clinical trial data to catalyze anticancer discoveries, and the Global Healthy Living Foundation, a nonprofit organization committed to improving the lives of individuals affected by serious and chronic health conditions. Partnering organizations that have developed immunotherapy resources for patients, caregivers, and providers included AIM at Melanoma, a global foundation aimed at curing melanoma, and Checkpoint NOW, a podcast series and website focused on practice guidelines and opinions about managing complex immune-related adverse events.
Focus of the Inaugural Meeting
During the inaugural sessions, physicians and other health-care professionals sat alongside patients, focusing on four high-priority areas: patient education and advocacy, reconsideration of the clinical definitions of immune-related adverse events, interventional clinical trials, and biomarker research. In the clinically based sessions, the Consortium discussed the dearth of patient support in terms of both educational material and the difficulty in finding others facing immune-related adverse events. The lack of a community and the need for education provided further momentum to launch a patient advocacy effort.
The other priority area in clinical care identified was the limitation of current classification systems for immune-related adverse events severity. The breakout sessions identified inadequate characterization of the impact on long-term organ function and quality of life for patients as a major limitation of the current Common Terminology Criteria for Adverse Events–based classifications, suggesting that modifications to upgrade the current system may be needed.

Identification of high-risk patients, strategies for safely co-managing these patients on immune checkpoint inhibitors, and the overall management of toxicities resulting from prolonged steroid tapering and optimization of immunomodulatory therapies were identified as key focus areas. These areas will guide both research and educational content development for clinicians, patients, and their caregivers In the field of experimental therapeutics, the think tank discussed pivotal ongoing trials in the field, including the ATRIUM trial, a phase III investigator-initiated study exploring whether abatacept reduces the risk of major adverse cardiovascular events compared with placebo in patients with immune checkpoint inhibitor–induced myocarditis (ClinicalTrials.gov identifier NCT05335928), and the AIM-NIVO trial, which is investigating nivolumab as a therapy for advanced or unresectable cancer in patients with preexisting autoimmune disorders (NCT03816345).
Regarding biomarker research, member institutions shared ongoing efforts in biobanking of specimens from patients who develop immune-related adverse events and reviewed current research in evaluating these data. Group discussion identified an imperative to establish uniform collection procedures to ensure the shareability of analyses. In this field, resource pooling and collaborative opportunities are crucial.
Moving Forward
Plans for continuing the work discussed at the inaugural irAE Consortium will go through two newly formed linked entities. ASPIRE will serve as the clinical and scientific consortium. In parallel, the patient advocacy arm will continue forward as STORIES.
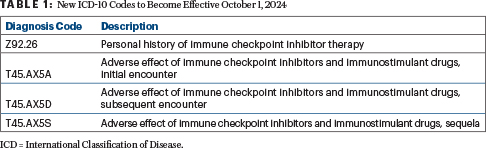
In its first landmark advocacy initiative, members of the ASPIRE and STORIES consortia paved the way for federal approval of specific International Classification of Disease (ICD) codes for immune-related adverse events, a critical advancement that has trailed behind the regulatory approval of immunotherapy. Clinicians currently use codes for autoimmune disease for billing while managing immune-related adverse events, thereby hampering precise attribution and identification and consequently obscuring accurate tracking of incidence and data analysis of these entities. Cofounding members recently submitted a proposal focusing on the need for accurate codes to ensure data integrity to the ICD-10 Coordination and Maintenance Committee, chaired by the Centers for Disease Control and Prevention as well as the Centers for Medicare and Medicaid Services. This proposal was granted approval with four new ICD-10 codes, which will become effective on October 1, 2024 (Table 1).
A networking session was held at the 2024 ASCO Annual Meeting on June 1 to engage diverse stakeholders in conversation. In addition, the ASPIRE consortium convenes quarterly in a virtual format to sustain its ongoing initiatives, complemented by an annual meeting, with the goal of advancing this field. Interested individuals and institutions are welcome to contact the authors for more information regarding future ASPIRE activities. The next annual ASPIRE and STORIES meeting is planned for February 28, 2025, to March 1, 2025, to be hosted by Duke University.
At this and future sessions, ASPIRE and STORIES will continue to generate thought-provoking discussion, brainstorm new therapeutic approaches, and inspire fresh collaborations around the new field of immune-related adverse events science and care.
DISCLOSURE: The authors are members of the irAE Consortium. Dr. Mittal has received honoraria from Aptitude Health, Cardinal Health, IntrinsiQ, Medpage, and Targeted Oncology; has served as a consultant or advisor to AstraZeneca, Aveo, Curio Science, Dendreon, Janssen, and Myovant; and has received research funding from Pfizer. Dr. Reynolds has served on an advisory board for SAGA Diagnostics; received speaker fees from MedScape and CMEOutfitters; and received institutional research funding from BMS. Dr. Funchain has received institutional research grants from Ideaya, BMS,Pfizer, and Taiho Oncology and personal fees from BMS, Merck, GigaGen, Eisai, Novartis, Array, Hexal AG, Replimune, and Immunocore.
Dr. Mittal is Assistant Professor of Medicine at UMass Chan Medical School in Worcester, Massachusetts, and Director of the GU Medical Oncology Section at UMass Memorial Medical Center. Dr. Reynolds is Assistant Professor Medicine at Harvard Medical School and Clinical Director of Inpatient Oncology Units and Director of the Severe Immunotherapy Complications Program at Massachusetts General Hospital, Boston. Dr. Funchain is Associate Professor of Medicine at Stanford University and Co-Director of both the Immunotherapy Toxicity Program and Skin Cancer Genomics Program at Stanford Cancer Institute in Stanford, California.

