GUEST EDITORS
Dr. Abutalib is Associate Director of the Hematology and Cellular Therapy Program and Director of the Clinical Apheresis Program at Cancer Treatment Centers of America, Zion, Illinois; Associate Professor at the Roseland Franklin University of Medicine and Science; and Founder and Co-Editor of Advances in Cell and Gene Therapy. Dr. Usmani is Chief of the Plasma Cell Disorders Division and Director of Clinical Research for Hematologic Malignancies, Department of Hematologic Oncology and Blood Disorders, Levine Cancer Institute/Atrium Health, Charlotte, North Carolina; and Clinical Professor of Medicine, UNC-Chapel Hill School of Medicine.

Syed Ali Abutalib, MD

Saad Z. Usmani, MD, FACP
The ASCO Post is pleased to present Hematology Expert Review, an ongoing feature that occasionally quizzes readers on issues in hematology. In this installment, Drs. Abutalib and Usmani consider unique considerations in the treatment of patients with cancer during the COVID-19 pandemic, focusing specifically on neutropenia, anemia, and thrombocytopenia. For each quiz question that follows, select the one best answer. The correct answers and accompanying discussions follow.
Question 1
In reference to the editorial published about COVID-19 in The New England Journal of Medicine, titled “Ten Weeks to Crush the Curve,”1 by Dr. Harvey V. Fineberg, which of the following statements is correct?
A. Everyone needs to be tested for COVID-19.
B. Everyone should be supplied with personal protective equipment.
C. Patients who were previously infected, have recovered, and are adequately immune may assist in the development, validation, and deployment of antibody-based tests.
D. Everyone does not need to wear a mask outside the home.
Question 2
According to the National Comprehensive Cancer Network (NCCN) Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to neutropenia-related considerations is correct?
A. Monitor patients in clinics at regular intervals to minimize emergency room visits.
B. Change the threshold for use of granulocyte-colony stimulating factor (G-CSF) in patients with regimens from only high-risk to intermediate-risk.
C. Do not use G-CSF in patients with neutropenic fever and COVID-19 infection.
D. Preference should be given to use of daily G-CSF administration over pegfilgrastim.
Question 3
According to the NCCN Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to anemia and erythropoietin-stimulating agents (ESAs), given the regional limited blood supply, is correct?
A. Red blood cell (RBC) transfusion should not be given to patients with a hemoglobin of 8 g/dL.
B. The panel suggests using the highest dose of ESA sufficient to avoid transfusion.
C. An increased risk of thrombosis has been observed with the use of ESAs.
D. All of the above.
Question 4
According to the NCCN Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to chemotherapy-associated thrombocytopenia, given the limited blood product supply, is correct?
A. For a nonbleeding patient, consider platelet transfusion once levels are between 15,000/mm3 and 20,000/mm3, despite the shortage of blood product supply.
B. There is an increased risk of thrombosis with thrombopoietin mimetics.
C. Consider cessation of thrombopoietin mimetics once platelet counts are above 30,000/mm3.
D. Consider initiation of thrombopoietin mimetics in patients with platelet counts of less than 100,000/mm3.
Question 5
In reference to the article published in The New England Journal of Medicine, titled “Fair Allocation of Scarce Medical Resources in the Time of COVID-19,”3 which of the following statements regarding the utility of resources for health-care providers during the COVID-19 pandemic is correct?
A. Asymptomatic health-care workers with COVID-19 infection should continue to work from their offices in a medical facility.
B. Allocation of scarce resources should be prioritized among patients infected with COVID-19 as opposed to patients with other serious medical condition(s).
C. Testing for COVID-19 should be prioritized for the most vulnerable populations.
D. Medical resources should be utilized based on a “first-come, first-served” model.
Answers to Hematology Expert Review Questions
Question 1
In reference to the editorial published about COVID-19 in The New England Journal of Medicine, titled “Ten Weeks to Crush the Curve,”1 by Dr. Harvey V. -Fineberg, which of the following statements is correct?
Correct answer: C. Patients who were previously infected, have recovered, and are adequately immune may assist in the development, validation, and deployment of antibody-based tests.
Expert Perspective
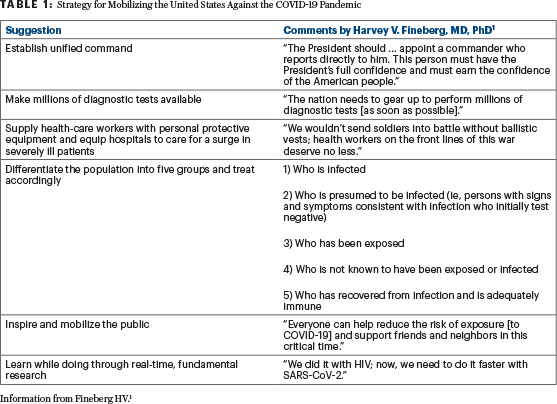
“The aim is not to flatten the curve; the goal is to crush the curve,” stated Harvey V. Fineberg, MD, PhD, of the Gordon and Betty Moore Foundation, Palo Alto, and the National Academies Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats, Washington, DC.1 According to Dr. Fineberg, this can be accomplished by the anniversary of D-Day in June 2020, the day America declares victory over the coronavirus, provided we immediately take six steps to mobilize and organize the nation (Table 1).1 Dr. Fineberg detailed the following necessary steps, dated April 23, 2020.1 Not everyone needs to be tested, but everyone with symptoms does need proper testing. We must supply health-care workers with personal protective equipment. Patients who were previously infected, have recovered, and are adequately immune may assist by the development, validation, and deployment of antibody-based tests. If everyone wears a surgical mask outside the home, those who are presymptomatic and infected will be less likely to spread the infection to others. During the COVID-19 pandemic, decisions to shape the public health response and to restart the economy should be guided by science. Also, we are in the process of learning the survival patterns of severe acute respiratory syndrome–coronavirus-2 under different environmental conditions and on various materials.1
Question 2
According to the NCCN Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to neutropenia-related considerations is correct?
Correct answer: B. Change the threshold for use of G-CSF in patients with regimens from only high-risk to intermediate-risk.
Expert Perspective
To minimize the incidence of neutropenic fever during the COVID-19 pandemic and achieve the goals of decreasing the clinic and emergency room (ER) visits and days of hospitalizations, the NCCN panel on hematopoietic growth factors suggests changing a few of the current recommendations with regard to neutropenic-related considerations, which include, but are not limited to, in the short-term to the following items:
The panel has changed the threshold for use of G-CSF in patients with regimens from only high-risk (> 20% risk of febrile neutropenia) to intermediate-risk (10%–20% risk of febrile neutropenia).
Expand the therapeutic use if patients previously not on G-CSF develop febrile neutropenia to include all patients, not just those with a risk factor for complications.
In the absence of long-acting G-CSF, consider self-administration of daily filgrastim instead of daily administration in the clinic.
The panel included a cautionary statement: “Physicians may wish to avoid use of or discontinue G-CSF in case of respiratory infection, respiratory symptoms, or confirmed or suspected COVID-19 to avoid increase in pulmonary inflammation or hypothetical risk of increasing inflammatory cytokines associated with adverse outcome.”
Question 3
According to the NCCN Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to anemia and erythropoietin-stimulating agents (ESAs), given the regional limited blood supply, is correct?
Correct answer: C. An increased risk of thrombosis has been observed with the use of ESAs.
Expert Perspective
Consider a “restrictive” threshold for RBC transfusion, eg, hemoglobin less than 7 g/dL, as has been studied in patients in intensive care units4 and those who have undergone hematopoietic cell transplantation.4 The threshold can be increased for patients with cardiopulmonary or other comorbid conditions. Currently, the guidelines for use of ESAs do not recommend use for 1) patients with cancer who are not on treatment; 2) those who are receiving minimally myelosuppressive regimens; or 3) those who are being treated with curative intent. Despite these recommendations, not all studies confirm reduced survival with use of ESAs in patients with cancer.2,5,6
Therefore, in light of the potential for blood shortages with the COVID-19 pandemic, the NCCN panel on hematopoietic growth factors suggests, for the short term, broadening the use of ESA therapy with or without intravenous iron supplementation to manage anemia in patients with malignancy requiring blood transfusion support. The panel suggests using the lowest dose of ESA sufficient to avoid transfusion. For example, hold the ESA for hemoglobin levels ≥ 10 g/dL. The panel included a cautionary statement: “An increased risk of thrombosis has been observed with use of ESAs.”
Question 4
According to the NCCN Short-Term Recommendations During COVID-19 Pandemic: Hematopoietic Growth Factors,2 which of the following statements with regard to chemotherapy-associated thrombocytopenia, given the limited blood product supply, is correct?
Correct answer: B. There is an increased risk of thrombosis with thrombopoietin mimetics.
Expert Perspective
Consider platelet transfusion in patients with thrombocytopenia less than 10,000/mm3 (some centers use up to 20,000/mm3 for outpatients2), modified for patients with bleeding.2 Consider thrombopoietin mimetics for patients with severe thrombocytopenia after chemotherapy (solid tumors7), start for platelet counts less than 30,000/mm3 to 50,000/mm3, and then discontinue for platelet counts above 75,000/mm3 to 100,000/mm3.2,7 The panel included a cautionary statement: “There is an increased risk of thrombosis with use of thrombopoietin mimetics.”
Question 5
In reference to the article published in The New England Journal of Medicine, titled “Fair Allocation of Scarce Medical Resources in the Time of COVID-19,”3 which of the following statements regarding the utility of resources for health-care providers during the COVID-19 pandemic is correct?
Correct answer: C. Testing for COVID-19 should be prioritized for the most vulnerable populations.
Expert Perspective
The choice to set limits on access to treatment is not a discretionary decision, but a necessary response to the overwhelming effects of a pandemic.3 Saving more lives and more years of life are consensus values across expert reports: Every life matters!
As physicians, nurses, or other health-care providers are incapacitated, all patients—not just those with COVID-19—will suffer greater mortality and years of life lost.8,9 First responders and health-care workers should be given priority, not because they are somehow more worthy, but because of their instrumental value: They are essential to pandemic response and saving more lives.
There should be no difference in allocating scarce resources between patients with COVID-19 and those with other serious medical condition(s).3 Epidemiologic modeling is even more relevant in setting priorities for COVID-19 testing. The Centers for Disease Control and Prevention currently gives priority to select groups of health-care workers and older (≥ 65 years) patients.10
A first-come, first-served approach is used for such resources as transplantable kidneys, where scarcity is long-standing and patients can survive without the scarce resource. Conversely, treatments for COVID-19 address urgent need, meaning a first-come, first-served approach would unfairly benefit patients living nearer to health facilities.3 First-come, first-served medication or vaccine distribution would encourage crowding and even violence during a period when social distancing is of paramount importance.3
DISCLOSURE: Dr. Abutalib is an advisor for AstraZeneca. Dr. Usmani has served as a consultant or advisor to AbbVie, Amgen, Celgene, GlaxoSmithKline, Janssen Oncology, Karyopharm Therapeutics, Seattle Genetics, SkylineDX, and Takeda; has participated in a speakers bureau for Amgen, Celgene, Janssen Oncology, and Takeda; has received research funding from Amgen, Array BioPharma, Bristol-Myers Squibb, Celgene, Janssen Oncology, Pharmacyclics, Sanofi, and Seattle Genetics.
REFERENCES
1. Fineberg HV: Ten weeks to crush the curve. N Engl J Med 382:e37, 2020.
2. National Comprehensive Cancer Network (NCCN): NCCN hematopoietic growth factors. Available at https://www.nccn.org/covid-19/pdf/HGF_COVID-19.pdf. Accessed May 21, 2020.
3. Emanuel EJ, Persad G, Upshur R, et al: Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med 382:2049-2055, 2020.
4. Tay J, Allan DS, Chatelain E, et al: Liberal vs restrictive red blood cell transfusion thresholds in hematopoietic cell transplantation: A randomized, open label, phase III, noninferiority trial. J Clin Oncol 38:1463-1473, 2020.
5. Aapro M, Leonard RC, Barnadas A, et al: Effect of once-weekly epoetin beta on survival in patients with metastatic breast cancer receiving anthracycline- and/or taxane-based chemotherapy: Results of the Breast Cancer–Anemia and the Value of Erythropoietin (BRAVE) Study. J Clin Oncol 26:592-598, 2008.
6. Ludwig H, Crawford J, Osterborg A, et al: Pooled analysis of individual patient-level data from all randomized, double-blind, placebo-controlled trials of darbepoetin alfa in the treatment of patients with chemotherapy-induced anemia. J Clin Oncol 27:2838-2847, 2009.
7. Soff GA, Miao Y, Bendheim G, et al: Romiplostim treatment of chemotherapy-induced thrombocytopenia. J Clin Oncol 37:2892-2898, 2019.
8. Wilson N, Kvalsvig A, Barnard LT, et al: Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis 26:1339-1441, 2020.
9. Gold J: Surging health care worker quarantines raise concerns as coronavirus spreads. Kaiser Health News, March 9, 2020. Available at https://khn.org/news/surging-health-care-worker-quarantines-raise-concerns-as-coronavirus-spreads/. Accessed May 21, 2020.
10. Centers for Disease Control and Prevention: Updated guidance on evaluating and testing persons for coronavirus disease 2019, March 8, 2020. Available at https://emergency.cdc.gov/han/2020/han00429.asp. Accessed May 21, 2020.

