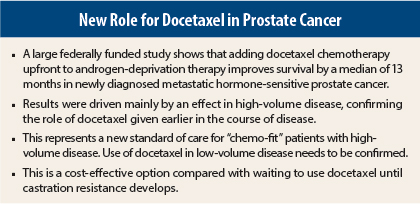
Adding docetaxel to standard androgen ablation therapy (ie, testosterone suppression) extended survival by more than 1 year in men with newly diagnosed metastatic hormone-sensitive prostate cancer in the phase III E3805 trial, funded by the National Institutes of Health. As reported at the ASCO Annual Meeting in Chicago,1 the survival benefit was observed mainly in men with more extensive metastatic disease.
ASCO Immediate Past President Clifford A. Hudis, MD, FACP, called these results achieved with an older drug “unprecedented” and “transformative.”
New Standard of Care
“We asked the question of whether you treat hormone-sensitive cancers more aggressively in the beginning or wait to add docetaxel,” said lead author Christopher J. Sweeney, MBBS, medical oncologist at the Lank Center of Genitourinary Oncology at the Dana-Farber Cancer Institute in Boston. “This is the first study to identify a strategy that prolongs survival in newly diagnosed metastatic prostate cancer. The benefit is substantial and warrants this being adopted as a new standard treatment for men who have high-extent disease and are able to tolerate chemotherapy,” he stated.
The E3805 study utilized two older therapies. Androgen-deprivation therapy has been used to treat prostate cancer for more than 50 years. Docetaxel transformed the landscape of treatment for prostate cancer when it was approved 10 years ago for the treatment of disease that has progressed on androgen-deprivation therapy (ie, castration-resistant prostate cancer). This study evaluated whether docetaxel can make a difference if given earlier in the course of disease, when the cancer is still hormone-sensitive.
From 2006 to 2012, E3805 enrolled 790 men with newly diagnosed metastatic prostate cancer and randomized them to androgen-deprivation therapy alone vs androgen-deprivation therapy plus six cycles of docetaxel. A preplanned interim analysis performed in October 2013 showed a significant improvement in survival with the addition of docetaxel. At the Annual Meeting, Dr. Sweeney presented updated overall survival results.
Median overall survival was significantly improved with the addition of docetaxel to androgen-deprivation therapy: 57.6 months vs 44 months for androgen-deprivation therapy alone (P = .0003), representing a 39% reduction in risk of death at every time point assessed. Deaths totaled 136 in the androgen-deprivation therapy–alone arm vs 101 in the androgen-deprivation therapy/docetaxel arm.
Greatest Benefit
Looking at the data in greater depth, most of the survival benefit was observed in men with extensive disease—either a high burden of bone metastases or liver or lung metastases. In that group (60% of study participants), median overall survival was 49.2 months for the combination vs 32.2 months for androgen-deprivation therapy alone (P = .0006), representing a 40% reduction in risk of death. In patients with low-volume disease, median overall survival has not yet been reached in either arm. Dr. Sweeney said that longer follow-up is needed to get more certainty on the benefit of docetaxel added to androgen-deprivation therapy in patients with low-volume metastatic disease.
Docetaxel delayed disease progression as assessed by prostate-specific antigen (PSA) or emergence of new metastases or symptom worsening. At 1 year, the percentage of patients with PSA < 2 ng/mL was 11.7% in the androgen-deprivation therapy group vs 22.7% in the androgen-deprivation therapy/docetaxel group (P < .0001). Median time to clinical progression was 19.8 months vs 32.7 months, respectively (P < .0001). Docetaxel also significantly improved median time to developing castration-resistant prostate cancer: 20.7 months vs 14.7 months for androgen-deprivation therapy alone (P < .0001).
Safety Profile
“It is feasible to administer docetaxel in this patient population,” Dr. Sweeney said. Nonhematologic toxicity and hematologic toxicity were consistent with what is described for docetaxel. Overall, 28% of patients had grade 3 or 4 events related to treatment.
The main toxicities associated with docetaxel were neutropenic fever (6%); sensory neuropathy (1%) and motor neuropathy (1%); and 1 of the 397 patients who received early docetaxel died due to treatment.
Quality-of-life data will be analyzed and presented at a later time.
At the press briefing where these findings were featured, Dr. Hudis praised the study. “This is an old drug and it reduces cost. I am not aware of another study that showed this magnitude of benefit in survival in sold tumors. This is an almost unprecedented improvement in survival.” ■
Disclosure: Dr. Sweeney reported a consulting or advisory role with Astellas Pharma, BIND Biosciences, Bionomics, Exelixis, Genentech, Janssen Pharmaceuticals, Roche, and Sanofi. For full disclosures of the study authors, visit abstracts.asco.org.
Reference
1. Sweeney C, Chen Y-H, Carducci MA, et al: Impact on overall survival with chemohormonal therapy versus hormonal therapy for hormone-sensitive newly metastatic prostate cancer: An ECOG-led phase III randomized trial. ASCO Annual Meeting. Abstract LBA2. Presented June 1, 2014.