In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
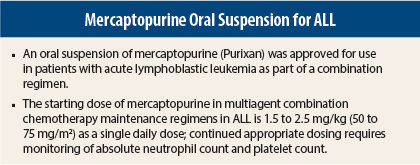
On April 28, 2014, an oral suspension of mercaptopurine (Purixan) was approved for use in patients with acute lymphoblastic leukemia (ALL) as part of a combination regimen.1,2 Mercaptopurine has been available only as a 50 mg tablet since its initial approval in 1953. Treatment of children with a 50-mg tablet is complicated by the ranges of age and weight that make body surface area dosing and dose adjustments difficult. Tablets also are not an ideal dosage form for children aged < 6 years.
The current formulation is a 20-mg/mL oral suspension, which offers the advantage of more accurate delivery of desired doses to children with a wide range of weights using a consistent administration schedule and more flexibility in dose adjustment. The commercially produced suspension is more likely to provide a more consistent dose of mercaptopurine than compounded formulations.
Pivotal Study
Approval was based on assessment of the bioequivalence of mercaptopurine from 50 mg Purinethol tablets and mercaptopurine from the oral suspension in a single-dose crossover clinical pharmacology study conducted in 62 healthy adult subjects under fasting conditions. Bioequivalence was demonstrated based on the primary pharmacokinetic parameters of area under the concentration-time curve (AUC)(0-t) and AUC(0-∞). Maximum concentration (Cmax) was not bioequivalent, with mean Cmax being 34% higher with the oral suspension.
Other clinical studies have shown that the absorption of an oral dose of mercaptopurine is incomplete and variable, averaging approximately 50% of the administered dose, and the factors affecting absorption are unknown. Following a single 50-mg dose of mercaptopurine oral suspension under fasting conditions, median AUC was 136 h*ng/mL (range = 74.2–264.8 h*ng/mL) and Cmax was 95 ng/mL (range = 39.5–204 ng/mL).
How It Works
Mercaptopurine activation occurs via hypoxanthine-guanine phosphoribosyl transferase (HGPRTase) and several enzymes to form 6-thioguanine nucleotides, incorporation of which into nucleic acids, instead of purine bases, results in cell-cycle arrest and cell death. Mercaptopurine competes with hypoxanthine and guanine for HGPRTase and is converted to thioinosinic acid. This intracellular nucleotide inhibits several reactions involving inosinic acid, including the conversion of inosinic acid to xanthylic acid and adenylic acid.
Methylation of thioinosinic acid produces 6-methylthioinosinate. Both have been reported to inhibit glutamine-5-phosphoribosylpyrophosphate amidotransferase, the first enzyme unique to the de novo pathway for purine ribonucleotide synthesis.
How It Is Given
The starting dose of mercaptopurine in multiagent combination chemotherapy maintenance regimens in ALL is 1.5 to 2.5 mg/kg (50 to 75 mg/m2) as a single daily dose. Continuation of appropriate dosing requires periodic monitoring of absolute neutrophil count and platelet count to assure sufficient drug exposure to maintain absolute neutrophil count at a desirable level and to adjust for excessive hematologic toxicity.
Patients with inherited little or no thiopurine S-methyltransferase (TPMT) activity are at increased risk for severe toxicity from conventional doses of mercaptopurine and generally require dose reduction. Testing for TPMT gene polymorphism should be considered in patients who experience severe bone marrow toxicities. Homozygous deficient patients may require a dose reduction of up to 90%. Most patients with heterozygous TPMT deficiency have tolerated recommended mercaptopurine doses, with some requiring dose reduction based on toxicities.
Safety Profile
Based on multicenter cooperative group ALL trials, the most common adverse events in > 20% of patients are anemia, neutropenia, lymphopenia, and thrombocytopenia. Adverse events occurring in 5% to 20% of patients include anorexia, nausea, vomiting, diarrhea, malaise, and rash. Rare adverse events occurring in < 5% include urticaria, hyperuricemia, oral lesions, elevated transaminases, hyperbilirubinemia, hyperpigmentation, and pancreatitis. Oral lesions resemble thrush rather than antifolic ulcerations.
Delayed or late toxicities include hepatic fibrosis, hyperbilirubinemia, alopecia, pulmonary fibrosis, oligospermia, and secondary malignancies. Drug fever has been rarely reported with mercaptopurine; every attempt should be made to exclude more common causes of pyrexia, such as sepsis, in patients with acute leukemia.
Mercaptopurine carries warnings/precautions for myelosuppression, hepatotoxicity, immunosuppression, and embryo-fetal toxicity. Complete blood count should be monitored and the mercaptopurine dose adjusted for severe neutropenia and thrombocytopenia. Patients with repeated severe myelosuppression should be evaluated for TPMT deficiency. Serum transaminase levels, alkaline phosphatase, and bilirubin levels should be monitored weekly at the start of therapy and monthly thereafter.
Due to immunosuppression associated with maintenance chemotherapy for ALL, response to all vaccines may be diminished and there is a risk of infection with live virus vaccines. Immunization guidelines for immunocompromised children should be consulted.
Report Adverse Events
Health-care professionals should report all serious adverse events suspected to be associated with the use of any medicine or device to FDA’s MedWatch Reporting System by completing a form online at www.fda.gov/medwatch/report.htm, by faxing (800-FDA-0178), by mailing the postage-paid address form provided online, or by telephone (800-FDA-1088). ■
References
1. U.S. Food and Drug Administration: Mercaptopurine. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm395156.htm.
2. PURIXAN™ (mercaptopurine) oral suspension prescribing information, NOVA Laboratories Limited, April 2014. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2014/205919s000lbl.pdf.