Question 1
Which of the following is one of the four major criteria for the diagnosis of essential thrombocythemia?
Correct Answer: A. Platelet count ≥ 450 × 109/L.
Expert Perspective
The diagnosis of essential thrombocythemia requires that all four major criteria or the first three major criteria (as shown in Table 1) plus a minor criterion are met to exclude other neoplastic and nonmalignant causes of thrombocytosis.1 Only choice A is a major criterion in this question. Choice C refers to a clonal marker other than mutation in JAK2, CALR, or MPL, for example, a clonal karyotype or molecular aberration. Bone marrow biopsy is particularly helpful in excluding other myeloid neoplasms associated with thrombocytosis, such as myelodysplastic syndromes associated with isolated del(5q), myelodysplastic/ myeloproliferative neoplasm with ringed sideroblasts and thrombocytosis, and in particular preprimary myelofibrosis.
__________________________________________________________________
TABLE 1: DIAGNOSTIC CRITERIA FOR ESSENTIAL THROMBOCYTHEMIA
The diagnosis of essential thrombocythemia requires that all major criteria or the first three major criteria plus the minor criterion are met.
Major Criteria
(1) Sustained platelet count ≥ 450 × 109 /L in the peripheral blood
(2) Bone marrow biopsy showing proliferation mainly of the megakaryocytic lineage, with increased numbers of enlarged, mature megakaryocytes with hyperlobulated nuclei; no significant increase or left shift in neutrophil granulopoiesis or erythropoiesis; rarely a minor (grade 1a) increase in reticulin fibrosis
(3) WHO criteria for BCR-ABL1–positive chronic myeloid leukemia, polycythemia vera, primary myelofibrosis, or other myeloid neoplasms are not met.
(4) JAK2, CALR, or MPL mutation
Minor Criteria
(1) Presence of a clonal marker (other than gene mutations listed in #4 major criterion)
(2) Absence of reactive thrombocytosis
WHO = World Health Organization.
Source: Thiele J, et al.1
_______________________________________________________________________________
Question 2
Approximately what percentage of essential thrombocythemia cases are triple-negative for JAK2, CALR, or MPL mutations?
Correct Answer: A. 12%.
Expert Perspective
Most WHO-defined essential thrombocythemia cases harbor a phenotypic driver mutation in JAK2 V617F (in ~50%–60% of cases), CALR (in ~30%), or MPL (in ~3%); about 12% of cases are triple-negative for these mutations.1-4 None of these mutations is specific for the diagnosis of essential thrombocythemia, but their presence excludes a reactive cause of thrombocytosis.1 It is noteworthy that a subset of triple-negative cases has been found to have gain-of-function mutations (eg, MPL S204P and MPL Y591N) through whole-exome sequencing or other sensitive molecular techniques.5,6 Such a finding is consistent with the assumption that JAK2/CALR/ MPL-wildtype essential thrombocythemia is not a homogeneous entity and that cases with polyclonal hematopoiesis probably constitute a hereditary disorder.6
Question 3
Which major peripheral blood smear abnormality is generally seen in essential thrombocythemia?
Correct Answer: B. Marked thrombocytosis.
Expert Perspective
The major abnormality seen in the peripheral blood of patients with essential thrombocythemia is marked thrombocytosis.1 The platelets often display anisocytosis, ranging from tiny forms to atypical large or giant platelets. Bizarre shapes, pseudopods, and agranular platelets may be seen, but they are uncommon. In WHO-defined essential thrombocythemia, the white blood cell count and leukocyte differential count are usually normal, although a borderline elevation in the white blood cell count may occur.1 The red blood cells are generally normocytic and normochromic, unless recurrent hemorrhage due to essential thrombocythemia (or from some other etiology) has caused iron deficiency, in which case they may be microcytic and hypochromic. Leukoerythroblastosis and teardrop-shaped red blood cells are not seen in essential thrombocythemia.1,7
Question 4
Which bone marrow abnormality is commonly observed in essential thrombocythemia?
Correct Answer: C. Marked proliferation of megakaryocytes dispersed throughout the bone marrow.
Expert Perspective
Hematopoietic cellularity is normal in most cases1,8 (Figure 1), but a small proportion of cases show a hypercellular bone marrow.1,9
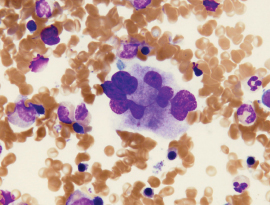
FIGURE 1: Large megakaryocyte with hyperlobulated nucleus in a bone marrow aspirate smear.
The most striking abnormality in the bone marrow is a marked proliferation of megakaryocytes, with a predominance of large to giant forms displaying abundant, mature cytoplasm and deeply lobed and hypersegmented (staghorn-like) nuclei1 (Figures 2 and 3).
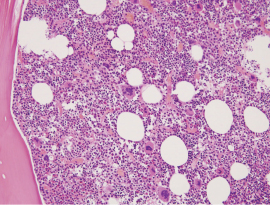
FIGURE 2: Bone marrow biopsy is mildly hypercellular, with an increased number of megakaryocytes.
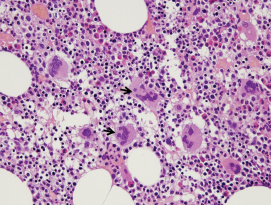
FIGURE 3: Megakaryocytes are increased in number and are large with hyperlobulated nuclei and some with a “staghorn” appearance (arrows) in the bone marrow biopsy. There is no increased proliferation of granulocytic or erythroid precursors.
The megakaryocytes are typically dispersed throughout the bone marrow, but they may occur in loose clusters.1 Unlike cases of preprimary myelofibrosis and primary myelofibrosis, the bizarre, highly atypical megakaryocytes or large dense clusters of megakaryocytes typically seen in these diseases are rarely found in essential thrombocythemia; if they are present, the diagnosis of essential thrombocythemia should be reconsidered.1,10
Question 5
Which of the following statements about bone marrow findings in essential thrombocythemia is correct?
Correct Answer: C. The finding of combined granulocytic and erythroid proliferation is uncommon.
Expert Perspective
The network of reticulin fibers is usually normal or is rarely (in < 5% of cases) minimally increased (but never to more than WHO grade 1 [Table 1]).1,8 Infrequently, reticulin fibrosis may increase in sequential bone marrow biopsy examinations.1,11 The finding of significant reticulin fibrosis or any collagen fibrosis at presentation excludes the diagnosis of essential thrombocythemia.1 The finding of even a low degree of combined granulocytic and erythroid proliferation in the bone marrow biopsy should raise suspicion of the prodromal stage of polycythemia vera, and the finding of granulocytic proliferation associated with bizarre, highly atypical megakaryocytes should raise suspicion of preprimary myelofibrosis.1 The large megakaryocytes with hypersegmented nuclei seen in essential thrombocythemia (Figure 3) contrast with the medium-sized nonlobated megakaryocytes seen in myelodysplastic syndromes with isolated del(5q) and with the small, dysplastic megakaryocytes seen in acute myeloid leukemia or myelodysplastic syndromes with inv(3)(q21;q26.2) or t(3;3)(q21;q26.2).1 ■
Acknowledgment: Faiz Ahmed Hussain, MD, of the Department of Internal Medicine, Jackson Park Hospital, Chicago, assisted in preparing this review.
DISCLOSURE: Drs. Abutalib and Medeiros reported no conflicts of interest.
REFERENCES
1. Thiele J, Kvasnicka HM, Orazi A, et al: Essential thrombocythaemia, in Swerdlow SH, Campo E, Harris NL, et al (eds): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, pp 50-53. Lyon, France, International Agency for Research in Cancer, 2017.
2. Tefferi A: Novel mutations and their functional and clinical relevance in myeloproliferative neoplasms: JAK2, MPL, TET2, ASXL1, CBL, IDH and IKZF1. Leukemia 24:1128-1138, 2010.
3. Tefferi A, Guglielmelli P, Larson DR, et al: Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood 124:2507-2513, 2014.
4. Tefferi A, Vainchenker W: Myeloproliferative neoplasms: Molecular pathophysiology, essential clinical understanding, and treatment strategies. J Clin Oncol 29:573-582, 2011.
5. Cabagnols X, Favale F, Pasquier F, et al: Presence of atypical thrombopoietin receptor (MPL) mutations in triple-negative essential thrombocythemia patients. Blood 127:333-342, 2016.
6. Milosevic Feenstra JD, Nivarthi H, Gisslinger H, et al: Whole-exome sequencing identifies novel MPL and JAK2 mutations in triple-negative myeloproliferative neoplasms. Blood 127:325-332, 2016.
7. Barbui T, Thiele J, Passamonti F, et al: Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: An international study. J Clin Oncol 29:3179-3184, 2011.
8. Thiele J, Kvasnicka HM, Facchetti F, et al: European consensus on grading bone marrow fibrosis and assessment of cellularity. Haematologica 90:1128-1132, 2005.
9. Thiele J, Kvasnicka HM, Diehl V: Initial (latent) polycythemia vera with thrombocytosis mimicking essential thrombocythemia. Acta Haematol 113:213-219, 2005.
10. Thiele J, Kvasnicka HM: Clinicopathological criteria for differential diagnosis of thrombocythemias in various myeloproliferative disorders. Semin Thromb Hemost 32:219- 230, 2006.
11. Thiele J, Kvasnicka HM, Schmitt-Graeff A, et al: Follow-up examinations including sequential bone marrow biopsies in essential thrombocythemia: A retrospective clinicopathological study of 120 patients. Am J Hematol 70:283-291, 2002.