A new approach to treating myelofibrosis appears to be paying off, according to several studies presented at the 2011 ASCO Annual Meeting. Treatment with a novel JAK inhibitor called ruxolitinib demonstrated significant and sustained improvement in splenomegaly and overall quality of life, functioning, and symptoms in patients with myelofibrosis, according to results of the phase III COMFORT-II trial that compared ruxolitinib vs best available therapy. A separate phase III trial comparing ruxolitinib to placebo (COMFORT-I) showed similar superiority for the novel JAK inhibitor.
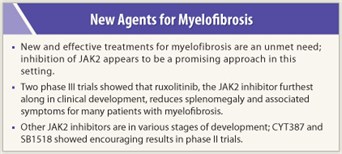
 Myelofibrosis, which encompasses a group of diseases involving scar tissue buildup in the bone marrow, can sometimes transform to leukemia. The disorder involves dysregulation of JAK-STAT signaling, and thus, trials to test the effect of JAK inhibition have been conducted. Phase I/II trials showed good activity for JAK2 inhibition with ruxolitinib (see “Early Clinical Findings with JAK2 Inhibition”), and two phase III trials were mounted: COMFORT-I (a placebo-controlled trial) and COMFORT-II (comparing ruxolitinib to best available therapy). At present, there are no FDA-approved agents for the treatment of myelofibrosis, but some drugs are used in this setting off-label.
Myelofibrosis, which encompasses a group of diseases involving scar tissue buildup in the bone marrow, can sometimes transform to leukemia. The disorder involves dysregulation of JAK-STAT signaling, and thus, trials to test the effect of JAK inhibition have been conducted. Phase I/II trials showed good activity for JAK2 inhibition with ruxolitinib (see “Early Clinical Findings with JAK2 Inhibition”), and two phase III trials were mounted: COMFORT-I (a placebo-controlled trial) and COMFORT-II (comparing ruxolitinib to best available therapy). At present, there are no FDA-approved agents for the treatment of myelofibrosis, but some drugs are used in this setting off-label.
“Data from both COMFORT trials may result in a new standard of care for a large number of patients with myelofibrosis,” said Claire Harrison, MD, Guy’s and St. Thomas’ NHS Foundation Trust, London, presenting author of COMFORT-II.
COMFORT-II
 COMFORT-II enrolled 219 patients with intermediate or high-risk primary myelofibrosis, post–essential thrombocythemia myelofibrosis, or post–polycythemia vera myelofibrosis and randomly assigned them in a 2:1 ratio to ruxolitinib at 15 or 20 mg twice daily vs best available therapy. The dose of ruxolitinib was determined by the patient’s platelet count. For the primary endpoint of achieving a 35% or greater reduction in spleen volume at week 48, ruxolitinib was significantly superior to best available therapy: 28.5% vs 0%, respectively (P < .0001). For the secondary endpoint (35% or greater reduction in spleen volume at week 24), ruxolitinib was also significantly superior to best available therapy: 31.9% vs 0%, respectively (P < .0001). Results showed that ruxolitinib significantly improved quality of life and symptoms associated with myelofibrosis from week 8 to week 48, as measured by the EORTC QLQ-C30 questionnaire. By contrast, the best available therapy group experienced progressive splenomegaly, worsening quality of life, and worsening symptoms over 48 weeks.
COMFORT-II enrolled 219 patients with intermediate or high-risk primary myelofibrosis, post–essential thrombocythemia myelofibrosis, or post–polycythemia vera myelofibrosis and randomly assigned them in a 2:1 ratio to ruxolitinib at 15 or 20 mg twice daily vs best available therapy. The dose of ruxolitinib was determined by the patient’s platelet count. For the primary endpoint of achieving a 35% or greater reduction in spleen volume at week 48, ruxolitinib was significantly superior to best available therapy: 28.5% vs 0%, respectively (P < .0001). For the secondary endpoint (35% or greater reduction in spleen volume at week 24), ruxolitinib was also significantly superior to best available therapy: 31.9% vs 0%, respectively (P < .0001). Results showed that ruxolitinib significantly improved quality of life and symptoms associated with myelofibrosis from week 8 to week 48, as measured by the EORTC QLQ-C30 questionnaire. By contrast, the best available therapy group experienced progressive splenomegaly, worsening quality of life, and worsening symptoms over 48 weeks.
Ruxolitinib had an acceptable safety profile compared with best available therapy. The most common adverse events were anemia and thrombocythemia.
COMFORT-I
 At the same ASCO session, COMFORT-I results were presented by Srdan Verstovsek, MD, PhD, of The University of Texas MD Anderson Cancer Center, Houston. COMFORT-I enrolled patients according to the same eligibility criteria as COMFORT-II and randomly assigned them to receive ruxolitinib vs placebo. At a median follow-up of 32 weeks, 41.9% of the ruxolitinib-treated patients vs 0.7% of the placebo group achieved the primary endpoint (ie, at least 35% shrinkage in spleen volume at week 24; P < .0001). Symptom burden was also significantly improved (P < .0001) with ruxolitinib vs placebo. More cases of thrombocythemia and anemia were observed in the ruxolitinib arm. ■
At the same ASCO session, COMFORT-I results were presented by Srdan Verstovsek, MD, PhD, of The University of Texas MD Anderson Cancer Center, Houston. COMFORT-I enrolled patients according to the same eligibility criteria as COMFORT-II and randomly assigned them to receive ruxolitinib vs placebo. At a median follow-up of 32 weeks, 41.9% of the ruxolitinib-treated patients vs 0.7% of the placebo group achieved the primary endpoint (ie, at least 35% shrinkage in spleen volume at week 24; P < .0001). Symptom burden was also significantly improved (P < .0001) with ruxolitinib vs placebo. More cases of thrombocythemia and anemia were observed in the ruxolitinib arm. ■
Disclosure: Dr. Harrison has served as a consultant for Celgene, Incyte, Novartis, S*BIO, and Shire. Dr. Verstovsek has conducted research for AstraZeneca, Bristol-Myers Squibb, Celgene, Geron, Incyte, Lilly, Roche, and S*BIO.
Expert Point of View: Novel JAK Inhibitor May Be an Option for Patients with Myelofibrosis
SIDEBAR: Early Clinical Findings with JAK2 Inhibition
References
1. Harrison C, et al: Results of a randomized study of the JAK inhibitor ruxolitinib (INC424) versus best available therapy (BAT) in primary myelofibrosis (PMF, post-polycythemia vera-myelofibrosis (PPV-MF), or post-essential thrombocythemia-myelofibrosis (PET-MF). 2011 ASCO Annual Meeting. Abstract LBA6501. Presented June 6, 2011.
2. Verstovsek S, Mesa RA, Gotlib JR, et al: Results of COMFORT-I, a randomized double-blind phase III trial of JAK 1/2 inhibitor INCB18424 (424) versus placebo (PB) for patients with myelofibrosis (MF). 2011 ASCO Annual Meeting. Abstract 6500. Presented June 6, 2011.

 Ross Levine, MD, of Memorial Sloan-Kettering Cancer Center, New York, was the discussant of the COMFORT-I and COMFORT-II trials.1 He explained that 70% to 90% of patients with myelofibrosis have JAK2 mutations, which appear to be endemic.
Ross Levine, MD, of Memorial Sloan-Kettering Cancer Center, New York, was the discussant of the COMFORT-I and COMFORT-II trials.1 He explained that 70% to 90% of patients with myelofibrosis have JAK2 mutations, which appear to be endemic.