In patients with triple-negative breast cancer who have residual disease after neoadjuvant chemotherapy, adjuvant capecitabine remains the standard of care. In the multicenter randomized noninferiority EA1131 trial, which included primarily basal tumors, noninferiority of adjuvant platinum over capecitabine could not be demonstrated, according to Ingrid A. Mayer, MD, MSCI, of Vanderbilt University, Nashville, who presented the findings at the 2021 ASCO Annual Meeting.1
“The available data show that platinum agents are unlikely to be noninferior or superior to capecitabine in improving invasive disease–free survival, regardless of intrinsic subtype,” Dr. Mayer said. “The study definitely reinforces the role of capecitabine in this high-risk group.”
Of note, the 3-year invasive disease–free survival rate was lower than expected, regardless of study treatment: 42% in the platinum arm and 49% in the capecitabine arm. In the CREATE-X trial, which established the value of adjuvant capecitabine for residual disease, the 5-year disease-free survival was 70% with capecitabine and 56% with observation.2

The available data show that platinum agents are unlikely to be noninferior or superior to capecitabine in improving invasive disease–free survival, regardless of intrinsic subtype.— Ingrid A. Mayer, MD, MSCI
Tweet this quote
“The event rate was much higher than expected, as the patient population we selected was at the highest possible risk,” Dr. Mayer explained. “Not only did 78% of participants have basal-like tumors—which have worse biologic behavior—but regarding residual disease, all patients had an RCB [residual cancer burden] score of 2 or 3. In CREATE-X, about 40% had an RCB score of 1.”
It is important to evaluate novel approaches in such a high-risk population, she emphasized, because that is precisely the population most in need of better strategies. “We don’t know how much capecitabine is helping that high-risk group because we don’t have a real comparator. However, we don’t know how to do anything better. Thus, for now, capecitabine remains the standard of care for these high-risk patients, although better strategies are definitely needed.”
About EA1131
Patients with triple-negative breast cancer left with residual disease after neoadjuvant chemotherapy have a very high risk for recurrence that may be reduced by adjuvant capecitabine.2 In the basal intrinsic subtype, preclinical models support the use of platinum agents.3 EA1131 tested the hypothesis that, for this subtype of triple-negative disease, treatment with a platinum rather than capecitabine may improve the odds of not recurring, but it was not proven.
EA1131 enrolled 410 patients with clinical stage II or III triple-negative breast cancer with residual disease ≥ 1 cm in the surgical specimen (breast or nodes) after standard neoadjuvant chemotherapy. Using the PAM50 assay, the researchers found 78% of the patients had the basal subtype, and this subgroup constituted the primary analysis population. Most tumors were high grade, and approximately half the patients had lymph node involvement. Residual tumors were primarily ypT1 (approximately 37%) and ypT2 (44%).
KEY POINTS
- The randomized noninferiority EA1131 trial aimed to determine whether adjuvant treatment with a platinum may be better than capecitabine in patients with early triple-negative breast cancer and residual disease after neoadjuvant therapy.
- Preclinical models have suggested these tumors may be sensitive to platinum.
- The study could not demonstrate noninferiority or superiority of the platinum.
- The 3-year invasive disease–free survival rates were low with either treatment: 42% with platinum and 49% with capecitabine.
- Capecitabine remains the adjuvant treatment of choice in this population.
The study initially assigned patients randomly to a platinum agent or observation, but the trial was soon amended to include capecitabine as the control arm, based on the CREATE-X results. Patients received carboplatin AUC 6 or cisplatin at 75 mg/m2 every 3 weeks for four cycles or capecitabine (1,000 mg/m2 BID on days 1–14) every 3 weeks for six cycles. Radiotherapy prior to or after treatment could be given at the provider’s discretion and was required in some situations.
A noninferiority design (hazard ratio [HR] noninferiority margin of 1.154) with a superiority alternative (alternative HR of 0.754) was chosen, assuming a 4-year invasive disease–free survival of 67% for the capecitabine arm. Noninferiority was tested first. If noninferiority was shown, a formal test for superiority of the platinum compared with capecitabine would be conducted.
At the fifth interim analysis, the hazard ratio for platinum/capecitabine was 1.09 (95% repeated confidence interval [CI] = 0.62–1.90), and the observed outcome in EA1131 was deemed “inconclusive.” Therefore, the data safety and monitoring committee recommended stopping the trial in March 2021, since it was unlikely to show noninferiority or superiority of the platinum arm and the grade 3 and 4 toxicities were more common with platinum agents.
Noninferiority Not Proven
“For patients with triple-negative breast cancer and residual disease after preoperative taxane plus anthracycline chemotherapy, the results of EA1131 suggest there is no role for adjuvant platinum agents,” Dr. Mayer reported.
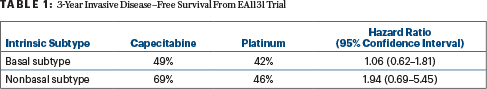
After a median follow-up of 20 months, 120 invasive disease–free survival events had occurred among the basal subtype cohort, including 90 distant recurrences and 15 locoregional recurrences. Their 3-year invasive disease–free survival rates were 42% with adjuvant platinum (95% CI = 30%–53%) and 49% (95% CI = 39%–59%) with adjuvant capecitabine (HR for platinum vs capecitabine = 1.06 [95% repeated CI = 0.62–1.81]). By intrinsic subtype, the 3-year invasive disease–free survival was 46% (95% CI = 38.1%–53.2%) for the basal subtype and 55% (95% CI = 38.6%–69.5%) for the nonbasal subtype, Dr. Mayer reported.
For the basal subtype, recurrence-free survival at 3 years was 46% with platinum and 49% with capecitabine (Table 1), and overall survival was 58% and 66%, respectively, she added.
Overall toxicity rates were similar in both arms (82%), but there were more severe hematologic adverse events with platinum agents, including grade ≥ 3 anemia (7% vs 0%) and leukopenia (10% vs 3%). Overall grade ≥ 3 adverse events were observed in 25% vs 15%. No deaths related to treatment were reported.
The main reason for early platinum discontinuation was the occurrence of adverse events (n = 21), whereas most patients discontinued capecitabine early for disease progression (n = 22).
Adjuvant Platinum Remains Experimental
“The adjuvant use of platinum agents in addition to taxane/anthracycline chemotherapy after upfront surgery remains investigational, and adjuvant trials with survival as the primary endpoint are ongoing (NRG BR-003). Better strategies are needed,” Dr. Mayer said.
The investigators are now performing correlative analyses of residual tissue; they are correlating surgical tissue profiling, circulating tumor cells, and cell-free DNA with recurrence-free survival and collecting patient-reported outcomes. “EA1131 provides a richly annotated biobank for discovery efforts,” she added.
DISCLOSURE: Dr. Mayer has served as a consultant or advisor to AbbVie, AstraZeneca, Blueprint Medicines, Cyclacel, Genentech, GlaxoSmithKline, Immunomedics, Lilly, MacroGenics, Novartis, Pfizer, Puma Biotechnology, and Seattle Genetics; and has received institutional research funding from Genentech, Novartis, and Pfizer.
REFERENCES
1. Mayer IA, Zhao F, Arteaga CL, et al: A randomized phase III post-operative trial of platinum-based chemotherapy versus capecitabine in patients with residual triple-negative breast cancer following neoadjuvant chemotherapy: ECOG-ACRIN EA1131. 2021 ASCO Annual Meeting. Abstract 605. Presented June 6, 2021.
2. Masuda N, Lee SJ, Ohtani S, et al: Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 376:2147-2159, 2017.
3. Lehmann BD, Bauer JA, Chen X, et al: Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121:2750-2767, 2011.

