In the phase I KEYNOTE-001 trial reported in The New England Journal of Medicine,1 Edward B. Garon, MD, of the David Geffen School of Medicine at the University of California, Los Angeles, and colleagues found that the programmed cell death protein 1 (PD-1) inhibitor pembrolizumab (Keytruda) produced durable responses in patients with advanced non–small cell lung cancer (NSCLC). Response rate and progression-free survival were increased in patients with higher levels of PD-1 ligand 1 (PD-L1).
Study Details
In the study, 495 patients received at least one dose of pembrolizumab between May 2012 and February 2014. Patients were assigned to a dose of 2 mg (n = 6) or 10 mg/kg (n = 287) every 3 weeks or 10 mg/kg every 2 weeks (n = 202) in either a training group (n = 182) or a validation group (n = 313).
PD-L1 expression was measured in tumor samples using immunohistochemical analysis; a proportion score was generated using the percentage of neoplastic cells with staining for membranous PD-L1. Response was assessed by central review every 9 weeks.
Among all patients: median age was 64 years; 53% were male; 82% were white; 35% and 64% had Eastern Cooperative Oncology Group performance status of 0 and 1; EGFR mutation was present in 15%, KRAS mutation in 26%, and ALK alteration in 2%; histology was nonsquamous in 81%; 24%, 21%, and 21% had received two, three, and at least four prior systemic therapies; 10% had a history of brain metastases; and 25% were never-smokers.
Outcome in All Patients
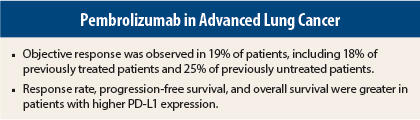
At the time of data cutoff, median duration of follow-up was 10.9 months (range = 5.2–27.5 months), and 115 patients (23%) continued to receive treatment. Among all patients, the objective response rate was 19.4% (95% confidence interval [CI] = 16.0%–23.2%), including 18.0% (95% CI = 14.4%–22.2%) in 394 previously treated patients and 24.8% (95% CI = 16.7%–34.3%) in 101 previously untreated patients. Stable disease was observed in 21.8% of patients.
Response rate was similar irrespective of dose, schedule, or histology. Current or former smokers had a higher response rate than never-smokers (22.5% vs 10.3%).
At the time of analysis, 84.4% of patients with a response had no disease progression. Median duration of response was 12.5 months (range = 1.0–23.3 months) in all patients, including 10.4 months (range = 1.0–10.4 months) in previously treated patients and 23.3 months (range = 1.0–23.3 months) in previously untreated patients.
Median progression-free survival was 3.7 months (95% CI = 2.9–4.1 months) among all patients, including 3.0 months (95% CI = 2.2–4.0 months) in previously treated patients and 6.0 months (95% CI = 4.1–8.6 months) in previously untreated patients. Median overall survival was 12.0 months (95% CI = 9.3–14.7 months) among all the patients, including 9.3 months (95% CI = 8.4–12.4 months) in previously treated patients and 16.2 months (95% CI = 16.2 months to not reached) in previously untreated patients.
Patients With High PD-L1 Expression
PD-L1 expression in ≥ 50% of tumor cells was selected as the proportion score cutoff for high expression in analysis of the training group. Among 824 samples from the total of 1,143 patients screened for the trial, PD-L1 proportion scores were ≥ 50% in 23.2%, 1% to 49% in 37.6%, and < 1% in 39.2%, with proportion scores ≥ 50% in 24.9% of previously untreated patients and 22.7% of previously treated patients.
In the validation group, PD-L1 status could not be assessed in 83 patients. In the remainder, the objective response rate was 45.2% (95% CI = 33.5%–57.3%) in 73 patients with a proportion score ≥ 50%, including rates of 43.9% (95% CI = 30.7%–57.6%) in previously treated patients and 50.0% (95% CI = 24.7%–75.3%) in previously untreated patients. No marked difference in response rate was observed according to dose, schedule, or smoking status in patients with a proportion score ≥ 50%.
Among 356 evaluable patients in the training and validation groups, PD-L1 expression proportion scores were ≥ 50% in 119, 1% to 49% in 161, and < 1% in 76. Median progression-free survival among patients with a proportion score ≥ 50% was 6.3 months (95% CI = 2.9–12.5 months) among all patients, including 6.1 months (95% CI = 2.1–12.5 months) in 294 previously treated patients and 12.5 months (95% CI = 2.4–12.5 months) in 62 previously untreated patients. Median overall survival among patients with a proportion score ≥ 50% was not reached in all patients (95% CI = 13.7 months to not reached), in previously treated patients (95% CI = 9.3 months to not reached), or in previously untreated patients (95% CI = not reached to not reached).
Adverse Events
The most common treatment-related adverse events of any grade were fatigue (19%), pruritus (11%), and decreased appetite (11%), with no clear difference according to dose or schedule. Treatment-related grade ≥ 3 adverse events occurred in 9.5% of patients, with the most common being dyspnea (3.8%) and pneumonitis (1.8%). Treatment-related inflammatory or immune-mediated adverse events occurring in > 2% of patients consisted of infusion-related reactions (3.0%), hypothyroidism (6.9%), and pneumonitis (3.6%).
Treatment discontinuation due to an infusion-related reaction occurred in one patient. One patient died from treatment-related pneumonitis.
The investigators concluded: “[W]e have shown the efficacy and safety of pembrolizumab for previously treated and previously untreated patients with non–small-cell lung cancer. Prospective testing of PD-L1 expression is feasible and retrospectively identified patients with an enhanced likelihood of having a clinical benefit from treatment with pembrolizumab.” ■
Disclosure: The study was funded by Merck. For full disclosures of the study authors, visit www.nejm.org.
Reference
1. Garon EB, Rizvi NA, Hui R, et al: Pembrolizumab for the treatment of non–small-cell lung cancer. N Engl J Med 372:2018-2028, 2015.