An emerging JAK inhibitor, pacritinib, appears not only effective in a broad population of patients with myelofibrosis but also among a subset with very low platelet counts, investigators from the global phase III PERSIST-1 trial reported at the 2015 ASCO Annual Meeting.1
“There is a huge unmet clinical need for patients with myelofibrosis,” said Ruben A. Mesa, MD, Deputy Director of the Mayo Clinic Cancer Center, Scottsdale, Arizona. “Symptoms of myelofibrosis have a substantial negative impact on both patient quality of life and overall survival.”
This need is especially felt among patients with very low platelet counts (< 50,000/µL), who tend to have shorter survival and are at increased risk for leukemic transformation. The one Food and Drug Administration (FDA)-approved agent, the JAK inhibitor ruxolitinib (Jakafi), is not considered safe for patients with low platelet counts, Dr. Mesa indicated. “There’s nothing for this population that is really efficacious,” he noted. “Individuals with counts < 50,000/µL are likely getting it in modest doses that probably impact efficacy.”
Pacritinib inhibits JAK2 and FLT3, whereas ruxolitinib inhibits JAK1 and JAK2. The drugs also have different effects on cytokines and on the spleen, he explained.
“Current treatments have not demonstrated the ability to simultaneously improve splenomegaly, symptoms, and cytopenias in myelofibrosis patients,” he pointed out.
“Pacritinib has activity in persons who do not have current treatments available, in particular, those with significant thrombocytopenia,” he said. “The endpoint with pacritinib was vastly superior in both the intent-to-treat and evaluable treatment arms. There were no responders in the best available treatment arm. The efficacy was similar in the broader group with < 100,000/µL.”
PERSIST-1 Details
The phase III PERSIST-1 trial enrolled 327 patients with myelofibrosis (primary myelofibrosis, post-polycythemia vera myelofibrosis, post-essential thrombocythemia myelofibrosis), randomizing them to pacritinib or “best alternative therapy,” which included a range of off-label treatments. These treatments did not include ruxolitinib due to safety concerns in patients with very low platelet counts, who were part of the study population. Patients in the study had not previously received ruxolitinib.
The primary endpoint was the proportion of patients achieving at least a 35% spleen volume reduction at week 24 by centrally reviewed magnetic resonance imaging or computed tomography. Secondary endpoints included the proportion achieving at least a 50% reduction in total symptom score at 24 weeks using the Myeloproliferative Neoplasm Symptom Assessment Form.
In this population, 32% of patients had a platelet count < 100,000/µL, and 15% had a platelet count < 50,000/µL; 75% were JAK2 V617F-positive.
The median duration of treatment was 16.2 months in the pacritinib arm and 5.9 months with the best available treatment. In the control arm, 74.5% received active treatment in the control arm (25.5% were watch and wait), including erythropoietin-stimulating agents, immunomodulatory drugs, hydroxyurea, and others.
Primary Endpoint Met
“This study demonstrated that pacritinib was well tolerated and induced significant and sustained spleen volume reduction and symptom control, even in patients with severe thrombocytopenia,” Dr. Mesa reported. “Pacritinib therapy also resulted in red blood cell transfusion independence in a significant proportion of patients.”
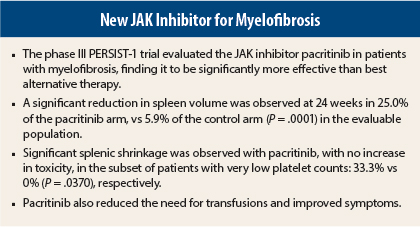
At 24 weeks, significant spleen shrinkage was observed in 19.1% of the pacritinib arm, compared with only 4.7% of the control arm (P = .0003), in the intent-to-treat analysis, and in 25.0% vs 5.9% (P = .0001) of the evaluable population (who both had baseline and 24-week assessments).
Additional Benefits
In other endpoints, additional benefits were observed with pacritinib, as described here for the evaluable patient population:
- Among patients with the lowest platelet counts, spleen shrinkage of at least 35% was observed in 33.3% vs 0% (P = .0370);
- Among patients dependent on red blood cell transfusions, transfusion independence was achieved by 25.7% vs 0% (P = .04);
- Among all patients, a significant reduction (at least 50%) in Total Symptom Score at 24 weeks was observed in 40.9% vs 9.9% (P < .0001);
- In the very low platelet subset, this reduction in symptoms was observed in 31.8% vs 11.1% (P = .3791).
Overall survival data are premature, but a landmark analysis at week 24 found that spleen shrinkage was associated with improved survival in the pacritinib arm but not in the control arm. “This highlights the importance of splenic reduction in impacting outcomes,” according to Dr. Mesa.
The most common toxicities with pacritinib were diarrhea, nausea, and vomiting, which were generally mild and resolved within 1 week. Few patients discontinued the drug due to side effects.
The ongoing phase III PERSIST-2 trial is exploring pacritinib in patients with low platelet counts due to their disease or therapy. ■
Disclosure: The study received funding from CTI BioPharma Corp. Dr. Mesa has received honoraria from and served as a consultant or advisor to Novartis and also has received research funding from Celgene, CTI, Gilead Sciences, and Incyte.
Reference
1. Mesa RA, Egyed M, Szoke A, et al: Results of the PERSIST-1 phase III study of pacritinib versus best available therapy in primary myelofibrosis, post-polycythemia vera myelofibrosis, or post-essential thrombocythemia-myelofibrosis. 2015 ASCO Annual Meeting. Abstract LBA7006. Presented May 30, 2015.