In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
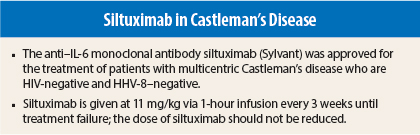
On April 23, 2014, the anti–interleukin (IL)-6 monoclonal antibody siltuximab (Sylvant) was approved for the treatment of patients with multicentric Castleman’s disease (a rare lymphoproliferative disorder) who are human immunodeficiency virus (HIV)-negative and human herpes virus (HHV)-8–negative.1,2 Approval was based on the finding of durable tumor and symptomatic response and complete resolution or stabilization of disease symptoms in an international phase II study.2 Siltuximab has not been studied in patients who are HIV-positive or HHV-8–positive because it did not bind to virally produced IL-6 in a preclinical study.
Pivotal Study
In the study, 79 patients were randomly assigned 2:1 to receive siltuximab at 11 mg/kg via intravenous infusion every 3 weeks plus best supportive care (n = 53) or placebo plus best supportive care (n = 26). Patients had a median age of 48 years (range = 20–78 years), 66% were male, 48% were Asian, and 39% were white. Histologic disease subtypes, which were similar in both groups, consisted of hyaline vascular subtype in 33%, plasmacytic in 23%, and mixed in 44%.
Treatment was continued until treatment failure (defined as disease progression based on increase in symptoms, radiologic progression, or deterioration in performance status) or unacceptable toxicity. Tumor response was assessed by independent review. A durable response was defined as a tumor and symptomatic response that persisted for a minimum of 18 weeks without treatment failure. For symptom response, 34 prospectively identified multicentric Castleman’s disease-related symptoms were graded by investigators.
Durable tumor and symptomatic response rates were 34% in the siltuximab group vs 0% in the placebo group (P = .0012). With regard to other prespecified endpoints, tumor response rates were 38% vs 4% (P < .05), median time to treatment failure after median follow-up of 422 days was not reached vs 134 days (hazard ratio = 0.418, P < .05). An increase in hemoglobin level of ≥ 1.5 g/dL at week 13 in patients who were anemic at study entry was observed in 19 vs 0 patients (P < .05).
How It Works
Siltuximab is a human-mouse chimeric anti–IL-6 monoclonal antibody. It binds to IL-6 and prevents the binding of IL-6 to both soluble and membrane-bound IL-6 receptors. IL6 is a cytokine with both proinflammatory and anti-inflammatory activities and is involved in numerous normal physiologic processes, such as induction of immunoglobulin secretion. Overproduction of IL-6 has been linked to systemic manifestations in patients with multicentric Castleman’s disease.
How It Is Given
Siltuximab is given at 11 mg/kg via 1-hour infusion every 3 weeks until treatment failure. The dose of siltuximab should not be reduced. Hematology tests must be performed prior to each dose for the first 12 months and every three dosing cycles thereafter. The absolute neutrophil count must be ≥ 1.0 × 109/L prior to initial administration and for retreatment, platelet count must be ≥ 75 × 109/L for initial treatment and ≥ 50 × 109/L for retreatment, and hemoglobin must be < 17 g/L for initial administration and retreatment. If hematologic criteria are not met, delay of treatment can be considered.
No initial dosage adjustment is necessary in patients with creatinine clearance ≥ 15 mL/min or mild-to-moderate hepatic impairment. The drug has not been studied in patients with end-stage renal disease or severe hepatic impairment.
Since CYP450 enzymes are downregulated by infection and inflammation stimuli including cytokines such as IL-6, inhibition of IL-6 by siltuximab may restore CYP450 activities to higher levels, leading to increased metabolism of drugs that are CYP450 substrates (eg, amiodarone, diazepam, omeprazole). In patients receiving CYP450 substrates with a narrow therapeutic index, therapeutic monitoring of effect (eg, warfarin) or drug concentration (eg, cyclosporine or theophylline) should be performed. The effect of siltuximab on CYP450 enzyme activity can persist for several weeks after stopping therapy.
Safety Profile
In the pivotal trial, siltuximab patients received a median of 19 infusions (range = 1–50 and placebo patients received a median of 8 (range = 2–32). Adverse event data reflect events occurring through the first eight infusions in the two groups. The most common adverse events of any grade in the siltuximab group were rash (28% vs 12% in the placebo group), pruritus (28% vs 8%), upper respiratory tract infection (26% vs 15%), edema (26% vs 27%), weight increase (19% vs 0%), and hyperuricemia (11% vs 0%). The most common grade 3 or 4 adverse events were edema (8% vs 0%), thrombocytopenia (4% vs 4%), and lower respiratory tract infection (4% vs 4%).
The safety of long-term administration in patients with multicentric Castleman’s disease was examined in 19 patients from an initial dose-finding study who benefited from continued treatment with 11 mg/kg every 3 to 6 weeks. Median exposure to siltuximab in these patients was 5.1 years (range = 3.4–7.2 years).
The most common adverse events of any grade were upper respiratory tract infection (63%), diarrhea (32%), pain in extremities, arthralgia, and fatigue (21% each). No patient discontinued therapy due to adverse events, there were no deaths, and no cumulative toxicities were identified. In overall experience with siltuximab, an anaphylactic reaction occurred in 1 of approximately 750 patients. Among 249 receiving siltuximab monotherapy, 4.8% have experienced infusion-related reactions.
The immunogenicity of siltuximab has been evaluated using an antigen-bridging enzyme immunoassay and an electrochemiluminescence-based immunoassay. Overall, anti-siltuximab antibodies have been found in 1 (0.2%) of 411 patients, with no neutralizing capability observed in the one case.
Siltuximab carries warnings/precautions for concurrent active severe infection, vaccinations, infusion-related reactions, and gastrointestinal perforation. Patients with severe infection should not receive siltuximab until the infection resolves, and all patients should be monitored closely for infection. Patients should not receive live vaccines, since IL-6 inhibition may interfere with the normal immune response. The drug should be permanently discontinued in patients with severe infusion-related reactions, anaphylaxis, severe allergic reactions, or cytokine release syndromes. ■
References
1. U.S. Food and Drug Administration: Approved drugs. Siltuximab. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm394675.htm.
2. SYLVANTTM (siltuximab) for Injection prescribing information, Janssen Biotech, Inc, April 2014. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2014/125496s000lbl.pdf.