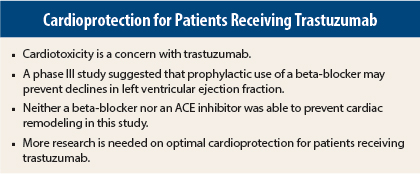
The beta-blocker bisoprolol was able to prevent trastuzumab (Herceptin)-associated declines in left-ventricular ejection fraction, whereas the effect of the angiotensin-converting–enzyme (ACE) inhibitor perindopril was less robust. Use of bisoprolol reduced dose interruptions for trastuzumab due to left-ventricular dysfunction and was safe. Despite the positive findings for bisoprolol, neither drug was able to prevent left-ventricular remodeling (as measured by left-ventricular end-diastolic volume) associated with trastuzumab therapy.
The MANTICORE (Multidisciplinary Approach to Novel Therapies in Cardiology Oncology Research) trial was designed to determine whether prophylactic use of a beta-blocker or an ACE inhibitor (two drugs used to treat established cardiovascular disease) could reduce trastuzumab-associated cardiotoxicity in patients with HER2-positive early breast. These results were presented at the 2015 San Antonio Breast Cancer Symposium.1
“To date, there have been no effective prevention strategies for trastuzumab-associated cardiotoxicity. Routine use of standard heart failure pharmacotherapy protects against trastuzumab-associated declines in left-ventricular ejection fraction and appears safe in HER2-overexpressing early breast cancer,” stated lead author Edith Pituskin, RN, PhD, of the University of Alberta in Edmonton.
HER2 is overexpressed in about 20% of all women with breast cancer, and trastuzumab reduces mortality by about one-third in women with HER2-positive breast cancer. All drugs come with risks and benefits, and cardiotoxicity is a concern with trastuzumab. About 20% of patients treated with trastuzumab experience left-ventricular dysfunction, and about 1%–5% develop heart failure.
Study Details and Results
The MANTICORE study was a three-arm 1:1:1 randomization, placebo-controlled, double-blind, multicenter trial that included 99 patients taking trastuzumab. At baseline, all patients had a left-ventricular ejection fraction ≥ 50%. Patients were randomized to receive bisoprolol, perindopril, or placebo during trastuzumab-based chemotherapy for 24 months. Cardiac magnetic resonance imaging parameters were assessed at baseline, at 3 months, at 12 months, and at 24 months. Accrual for the study was stopped after the first 99 patients were enrolled due to the low likelihood that additional participants would change the primary outcome.
Mean age at baseline was about 50 years. Anthracyclines, known to be cardiotoxic, were given (along with trastuzumab) to 23% of the placebo group, 33% of the perindopril group, and 12% of the bisoprolol group.
Bisoprolol significantly prevented reduction in left-ventricular ejection fraction from baseline vs placebo (P = .001) and also prevented trastuzumab interruptions due to drop in left-ventricular ejection fraction (P = .002). Post-treatment left-ventricular ejection fraction declined from 61% to 56% for placebo, from 62% to 59% for perindopril, and from 62% to 61% for bisoprolol.
A multivariate analysis showed that baseline left-ventricular ejection fraction and bisoprolol and perindopril were the only factors that affected left-ventricular ejection fraction during the study. ■
Disclosure: Dr. Pituskin reported no potential conflicts of interest.
Reference
1. Pituskin E, Mackey JR, Koshman S, et al: Prophylactic beta blockade preserves left ventricular ejection fraction in HER2-overexpressing breast cancer patients receiving trastuzumab: Primary results of the MANTICORE randomized, controlled trial. 2015 San Antonio Breast Cancer Symposium. Abstract S1-05. Presented December 9, 2015.