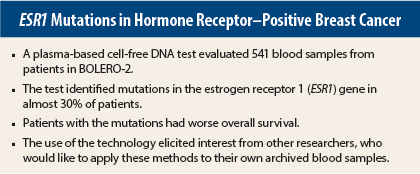
A plasma-based cell-free DNA test identified mutations in the estrogen receptor 1 gene (ESR1) in 30% of patients from the BOLERO-2 trial of everolimus (Afinitor) plus exemestane, and these mutations were correlated with survival. The results, which support the use of plasma as a source of prognostic—and perhaps predictive—information, were reported at the 2015 San Antonio Breast Cancer Symposium by Sarat Chandarlapaty, MD, of Memorial Sloan Kettering Cancer Center, New York.1
“Using a simple blood test, we found that the D538G and Y537S mutations in the estrogen receptor are more common in patients with advanced, estrogen receptor–positive breast cancer than previously appreciated,” Dr. Chandarlapaty revealed.
The findings were met with enthusiasm by researchers interested in correlative studies of clinical trials, including 2016 President-Elect of ASCO Daniel Hayes, MD. “These trials were started before we recognized the importance of plasma DNA, so I’m pretty certain these samples were not handled in a way that we all believe they should be,” said Dr. Hayes, the Stuart B. Padnos Professor of Breast Cancer Research and Co-Director of the Breast Oncology Program in the University of Michigan Comprehensive Cancer Center, Ann Arbor.
Dr. Hayes said during the discussion, “I am asking this, because if you did something special to the samples, the rest of the research world would like to know what it is. We are all sitting on samples that we have been told are worthless. Are we wrong?”
No, said Dr. Chandarlapaty, who noted that no unusual processing was involved in his analyses. “We collected these plasma samples, not thinking about doing genomic analyses for estrogen receptor mutations,” he said. Aside from performing “an additional hard spin,” he added, the handling of the samples was standard. “The results tell us that some of the archival samples in our freezers may be usable for analysis.”
Key Results
The analysis revealed two key mutations in the estrogen receptor 1 gene (ESR1), which they observed to be associated with survival of patients in the BOLERO-2 trial. “D538G and Y537S mutations appear to be associated with a more aggressive disease biology, as demonstrated by shorter overall survival. Patients with these mutations don’t respond as well to currently used therapies and die sooner than patients without these mutations,” Dr. Chandarlapaty reported.
The researchers conducted cell-free DNA testing on blood samples from 541 patients. Of them, 155 (28.8%) had the D538G and/or Y537S mutation; 83 (15.3%) had the D538G mutation; and 30 (5.5%) had both.
In an assessment of 302 archived solid tumor samples evaluated by next-generation sequencing, the ESR1 mutation was identified in only 3 (1.3%) of those samples.
Both D538G and Y537S mutations were associated with shorter overall survival. Median overall survival in BOLERO-2 was 32.1 months in patients without mutations, vs 20.7 months in patients with one or both mutations—a highly significant difference (P = .000037). In patients with both mutations, overall survival fell to 15.2 months. Risk related to the Y537S mutation was more than doubled, vs no mutation.
“In a multivariate analysis adjusting for sensitivity to prior hormonal therapy, visceral disease and ECOG [Eastern Cooperative Oncology Group] performance status, the effect of ESR1 mutation, compared to wild-type, on overall survival remained significant,” he added.
Referring to a previous mutational analysis of tumor specimens by Hortobagyi et al, which found no association between various mutations and treatment outcomes, he said, “I think plasma will identify this particular and critically important alteration better.”
Could ESR1 Be Predictive?
Further analyses, which Dr. Chandarlapaty emphasized are preliminary and hypothesis-generating only, revealed differences in how these two mutations affect response to everolimus. BOLERO-2 showed that adding everolimus to exemestane significantly reduced the risk of disease progression by 55% in metastatic patients who progressed after treatment with an aromatase inhibitor.2
“Patients with the D538G mutation derived a large benefit from the addition of everolimus, whereas those with the Y537S mutation did not,” he reported.
In the exemestane-only arm, median progression-free survival was 3.9 months in wild-type patients, 2.7 months in those with the D538G mutation, and 4.1 months in patients with the Y537S mutation. In the arm receiving exemestane plus everolimus, median survival increased to 8.5 months in wild-type patients and 5.8 months in those with the D538G mutation but remained stable at 4.2 months in those with the Y537S mutation.
The addition of everolimus, therefore, seems to confer no benefit over exemestane alone in the Y537S mutation group. “These unexpected results require further validation,” he added. ■
Disclosure: Dr. Chandarlapaty has consulted for Chugai, Foresite Capital, and Oncothyreon.
References
1. Chandarlapaty S, Sung P, Chen D, et al: cfDNA analysis from BOLERO-2 plasma samples identifies a high rate of ESR1 mutations: Exploratory analysis for prognostic and predictive correlation of mutations reveals different efficacy outcomes of endocrine-therapy-based regimens. 2015 San Antonio Breast Cancer Symposium. Abstract S2-07. Presented December 9, 2015.
2. Baselga J, Campone M, Piccart M, et a: Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366:520-529, 2012.