In a phase II trial reported in The New England Journal of Medicine by Jia Ruan, MD, PhD, and colleagues, first-line treatment with the immunomodulatory agent lenalidomide (Revlimid) and the anti-CD20 antibody rituximab (Rituxan) followed by maintenance lenalidomide and rituximab produced a high response rate, prolonged remission, and promising survival outcomes in patients with mantle cell lymphoma.1 Initial treatment of mantle cell lymphoma is not standardized but generally includes cytotoxic chemotherapy; cure is seldom achieved.
Study Details
In the single-group study, 38 patients enrolled at 4 U.S. sites between July 2011 and April 2014 received induction and maintenance treatment with lenalidomide and rituximab, During induction, lenalidomide was given at 20 mg daily (10 mg if creatinine clearance 30 to < 60 mL/min) on days 1 to 21 of 28-day cycles for 12 cycles, with the dose being escalated to 25 mg daily (15 mg) after the first cycle if no dose-limiting adverse events occurred during the first cycle. Rituximab was given at 375 mg/ m2 during weeks 1, 2, 3, 4, 13, 21, 29, 37, and 45, for a total of nine doses. Starting with cycle 13, maintenance lenalidomide was given at 15 mg (5 mg) daily on days 1 to 21 of 28-day cycles, while maintenance rituximab was given every other cycle. Treatment was continued for at least 36 cycles or until disease progression, development of unacceptable adverse effects, or withdrawal from the study.
Thromboprophylaxis with aspirin or low–molecular-weight heparin was administered to all patients unless treatment for known thrombosis was required. Asymptomatic hepatitis B virus carriers received antiviral therapy. Prophylactic growth factors were not empirically given. The primary endpoint was overall response rate.
Patients had a median age of 65 years (range, 42–86 years), 71% were male, 97% had an Eastern Cooperative Oncology Group performance status of 0 or 1, 100% had Ann Arbor stage III or IV disease, 39% had an elevated lactate dehydrogenase level, and 89% had bone marrow involvement. In addition, 34% had low-risk, 34% intermediate-risk, and 32% high-risk disease on Mantle Cell Lymphoma International Prognostic Index (MIPI) scores; 47% had low-intermediate risk, 26% had high-intermediate risk, and 11% had high-risk disease on the International Prognostic Index (IPI); and Ki67 index was < 30% in 68% and ≥ 30% in 21%. The most common indications for treatment were symptomatic lymphadenopathy (53%), cytopenias (18%), and bulky disease (13%).
Responses and Survival
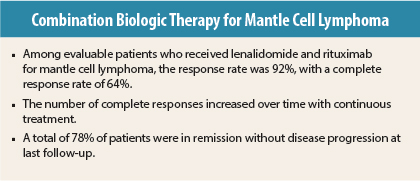
At a median follow-up of 30 months, the overall response rate among 36 evaluable patients was 92% (95% confidence interval [CI] = 78%–98%), with a complete response rate of 64% (95% CI = 46%–79%). The number of complete responses increased over time with continuous treatment. Median time to partial response was 3 months (range, 3–13) months, and median time to complete response was estimated at 11 months (range, 3–22 months).
Median progression-free survival and overall survival had not been reached. Two-year progression-free survival was 85% (95% CI = 67%–94%), and 2-year overall survival was 97% (95% CI = 79%–99%). MIPI and IPI scores and Ki67 index were not correlated with response or progression-free survival; high-risk disease on MIPI was associated with unfavorable overall survival (P = .05).
Among the 36 evaluable patients, 78% were in remission without disease progression at last analysis, including 26 who had completed induction therapy and were receiving maintenance therapy, 1 who had almost completed induction therapy, and 1 who had received study treatment for 3 years and was no longer receiving therapy while remaining in complete remission.
Adverse Events
For both treatment phases, the most common adverse events of any grade were neutropenia (74%) and anemia (60%) among hematologic adverse events and fatigue (74%), rash (66%), fever (58%), cough (55%), diarrhea (55%), and hyperglycemia (50%) among nonhematologic adverse events. Grade 1 or 2 infections included upper respiratory tract infection (39%), urinary tract infection (18%), and sinusitis (11%).
The most common grade 3 or 4 adverse events were neutropenia (50%), rash (29%), thrombocytopenia (13%), an inflammatory syndrome (“tumor flare”; 11%), and anemia (11%). Secondary cancers were observed, consisting primarily of noninvasive skin cancers requiring local therapy, including squamous cell carcinoma in two patients, basal cell carcinoma in one patient, and melanoma in situ in two patients. Merkel cell carcinoma developed in an 86-year-old patient after 18 months of treatment, and pancreatic cancer was diagnosed in a 68-year-old patient after 12 months of treatment.
Among the 33 patients with normal renal function, 36% had no unacceptable side effects associated with dose escalation from 20 mg to 25 mg, and 42% required a dose reduction from 20 mg to ≤ 15 mg. During induction therapy, rituximab was discontinued in two patients with serum sickness–like symptoms. During maintenance therapy, six patients received modified therapy during remission. Rituximab was discontinued in two patients with hypogammaglobulinemia, and lenalidomide was discontinued in four patients, due to investigator discretion for two patients, after asymptomatic grade 4 liver function abnormality in one patient, and due to a reversible grade 4 ventricular arrhythmia in a patient with a history of dysrhythmia.
Quality of life assessed by Functional Assessment of Cancer Therapy–Lymphoma (FACT-Lym) showed trends toward improvement among patients completing the instrument at baseline and month 12 (P = .04) and baseline and month 21 (P = .06).
The investigators concluded: “Combination biologic therapy consisting of lenalidomide plus rituximab was active as initial therapy for mantle cell lymphoma.” ■
Disclosure: The study was funded by Celgene and a Weill Cornell Medical College Clinical Translational Science Center grant. For full disclosures of the study authors, visit www.nejm.org.
Reference
1. Ruan J, Martin P, Shah B, et al: Lenalidomide plus rituximab as initial treatment for mantle-cell lymphoma. N Engl J Med 373:1835-1844, 2015.
See commentary by Michael Wang, MD, PhD, here.