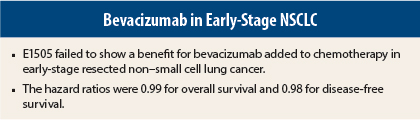
Overall survival in patients with surgically resected early-stage non–small cell lung cancer (NSCLC) did not improve with the addition of bevacizumab (Avastin) to chemotherapy, according to the findings of a study researchers have called a “top abstract” from the 16th World Conference on Lung Cancer.
Heather Wakelee, MD, Associate Professor of Medicine (Oncology) at Stanford University Medical Center, California, presented the phase III E1505 study results on behalf of the ECOG-ACRIN Cancer Research Group.1 She noted that bevacizuimab has been shown to improve outcomes when added to platinum-based chemotherapy in advanced-stage nonsquamous NSCLC. This study evaluated the drug in early-stage patients.
Study Details and Results
The study involved 1,501 patients with early-stage NSCLC (stage IB to IIIA, squamous and nonsquamous) whose tumors were resected between 2007 and 2013. Within 6 to 12 weeks of surgery, they were randomized to receive adjuvant chemotherapy or chemotherapy plus bevacizumab.
The chemotherapy regimen consisted of four cycles (every 3 weeks) of cisplatin (75 mg/m2) with vinorelbine, docetaxel, gemcitabine, or pemetrexed (Alimta) per physician’s choice. The experimental arm also received bevacizumab (15 mg/kg) every 3 weeks starting with cycle 1 of chemotherapy and continuing for 1 year. Postoperative radiation therapy was not permitted.
The study results were released early, due to futility, after the interim analysis at a median follow-up of 41 months.
Dr. Wakelee noted that 230 of 1,501 patients enrolled were ineligible, mostly because of inadequate nodal sampling. More than 80% completed all planned protocol treatment in the control arm, but after continued dropouts, only 37% completed the entire year of treatment in the bevacizumab arm.
“The addition of bevacizumab to adjuvant chemotherapy failed to improve survival for patients with surgically resected early-stage NSCLC,” Dr. Wakelee reported. The hazard ratio for median overall survival, the primary endpoint, was 0.99 (P = .93) and was 0.98 (P = .75) for disease-free survival. “There was absolutely no difference between the arms for the overall survival and disease-free survival curves,” she added.
‘Not the End of the Story’
In a press briefing, Dr. Wakelee said the failure of bevacizumab to show a benefit in early-stage disease was in keeping with what has been seen with the drug in colorectal cancer, where it also failed to show a benefit in the adjuvant setting.
Bevacizumab added no unexpected toxicities, but there was a significant increase in neutropenia and hypertension. Grades 3–5 toxicities that were significantly higher in the bevacizumab than in the control group included hypertension (30% vs 8%) and neutropenia (38% vs 33%). Overall grade 3 and higher adverse events were observed in 84% and 67%, respectively.
“The study highlights the importance of randomized trials to prove—or disprove—the utility of drugs in different stages of disease,” Dr. Wakelee said. “With the development of other active agents in metastatic lung cancer, it will be important to investigate them fully in earlier stages and not assume the benefit seen in advanced stage will also be proven in earlier stages, though we can remain hopeful.”
“This is not the end of the story,” she added. “We have many very important subset analyses to be done and a significant amount of correlative work, which hopefully will be very meaningful,” she said. ■
Disclosure: Dr. Wakelee is an unpaid consultant for Genentech/Roche.
Reference
1. Wakelee HA, Dahlberg SE, Keller SM, et al: Randomized phase III trial of adjuvant chemotherapy with or without bevacizumab in resected non-small cell lung cancer: Results of E1505. 16th World Conference on Lung Cancer: Abstract PLEN04.03. Presented September 9, 2015.