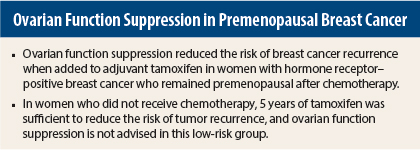
Results of the large International Breast Cancer Study Group (IBCSG)-coordinated SOFT trial present a convincing argument for the addition of ovarian function suppression to adjuvant hormonal therapy to reduce the risk of tumor recurrence in younger women with hormone receptor–positive early-stage breast cancer at high enough risk to be treated with chemotherapy and who remain premenopausal. Compared with tamoxifen alone, ovarian function suppression plus exemestane achieved a greater reduction in the risk of tumor recurrence than ovarian function suppression plus tamoxifen. In the cohort of premenopausal women younger than age 35, substantial benefits were seen with ovarian suppression.
In the cohort of women who had not received chemotherapy, tamoxifen alone was just as effective as tamoxifen plus ovarian function suppression. Thus, tamoxifen appears to be sufficient therapy to reduce the risk of tumor recurrence for premenopausal women with low-risk cancers not requiring chemotherapy. This group of premenopausal women was older with predominantly small node-negative tumors of low to intermediate grade.
Tamoxifen has been the standard of care for adjuvant therapy in premenopausal women with hormone receptor–positive early-stage breast cancer. Studies of ovarian function suppression have been equivocal in younger patients. The SOFT study was designed to address this issue by including only patients who retained or regained a premenopausal estradiol level after chemotherapy.
“I believe this trial is practice-changing. If I see a woman under age 35 with hormone receptor–positive breast cancer, I will know how to advise her. I also feel more comfortable with tamoxifen alone in an older premenopausal woman with a small, low-risk breast cancer,” stated lead author Prudence Francis, MD, Head of Breast Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia. She presented these results at the 2014 San Antonio Breast Cancer Symposium.1
Closer Look at the SOFT Trial
The SOFT trial was designed to assess the value of ovarian function suppression in 3,047 premenopausal women with hormone receptor–positive breast cancer treated for 5 years with tamoxifen plus ovarian function suppression vs tamoxifen alone or exemestane plus ovarian function suppression. Women randomly assigned to ovarian function suppression had the choice of 5 years of monthly injections of triptorelin (Trelstar), surgical removal of the ovaries, or radiation therapy to ovaries.
These treatments were compared in two different groups of women: women who had received prior adjuvant chemotherapy (53%) and women who did not receive chemotherapy (47%). The women who received chemotherapy were on average younger with higher-risk larger tumors that were more likely to be node-positive; the women who did not receive chemotherapy had low-risk tumors. Women who had chemotherapy entered the trial up to 8 months postchemotherapy, whereas those who had no chemotherapy entered the trial within 12 weeks after surgery.
The primary analysis was between tamoxifen vs tamoxifen plus ovarian function suppression. At a median follow-up of 5.6 years, there was no overall benefit for the addition of ovarian function suppression to tamoxifen; 5-year event-free survival was 84.7% with tamoxifen alone vs 86.6% for tamoxifen plus ovarian function suppression (P = NS).
However, in the cohort that remained premenopausal after chemotherapy (median age, 40 years), ovarian function suppression added to tamoxifen achieved a 22% reduction in the relative risk of tumor recurrence vs tamoxifen alone.
A secondary analysis showed that the combination of exemestane plus ovarian function suppression was even better in the premenopausal prior chemotherapy cohort, with a 35% relative risk reduction for tumor recurrence vs tamoxifen alone.
In the cohort of women who remained premenopausal after chemotherapy, the 5-year breast cancer–free interval was 78.0% for tamoxifen alone, 82.5% for tamoxifen plus ovarian function suppression, and 85.7% for exemestane plus ovarian function suppression.
“In women under age 35, approximately one in three women assigned tamoxifen alone had a tumor recurrence within 5 years compared with one in six for exemestane plus ovarian function suppression,” Dr. Francis stated.
The cohort of women who did not receive chemotherapy (median age, 46 years) did well in all three study arms. The 5-year breast cancer–free interval was 95.8% with tamoxifen alone, 95.1% with tamoxifen plus ovarian function suppression, and 97.1% with exemestane plus ovarian function suppression.
“In this older group of women who did not have chemotherapy, there is no reason to add ovarian function suppression. Their average age is 46 years, and some of these women will naturally go into menopause soon,” Dr. Francis said.
Quality of Life
Karin Ribi, PhD, a psychologist with the IBCSG, presented a separate analysis of patient-reported changes from baseline in endocrine symptoms, sexual function, and quality of life in SOFT participants.2
Mood and well-being did not differ between the three treatment arms. Endocrine symptoms were present in all three treatment arms. For the primary comparison, endocrine symptoms were initially worse with the combination of tamoxifen and ovarian function suppression compared with tamoxifen alone.
Sexual function was impacted in all three treatment arms. This parameter was worse in the tamoxifen plus ovarian function suppression arm compared with tamoxifen alone, as measured by patient-reported interest in sex, and was the worst in the exemestane plus ovarian function suppression arm, Dr. Ribi noted.
When these symptoms were analyzed according to whether patients received chemotherapy, treatment differences for endocrine symptoms and sexual function were less pronounced in those who previously had chemotherapy.
“Our hypothesis is that women treated with chemotherapy already had experienced side effects, and when they move to hormonal therapy, they already know they have a worse risk profile, so they may be more willing to accept these side effects,” Dr. Ribi suggested in an interview with The ASCO Post.
‘Convincing Data’
Commenting on the SOFT study, Carlos L. Arteaga, MD, Director of the Breast Cancer Program at Vanderbilt-Ingram Cancer Center in Nashville and President of the American Association for Cancer Research, said that he found these data convincing.
“This was a solid presentation. I am persuaded by the findings in women under 35, and I was impressed by the clear separation between the curves. Perhaps the most important aspect of this study is that the researchers included only women who were premenopausal at the start of the study, whereas this was not true of other studies of ovarian function suppression,” he said.
Questions Remain
The formal discussant of this trial, Hope S. Rugo, MD, of the University of California, San Francisco, said that the biggest question for treatment of premenopausal hormone-sensitive breast cancer is “how much [ovarian suppression] is enough.”
“If we use ovarian function suppression should we use tamoxifen or an aromatase inhibitor? In whom should we avoid chemotherapy? We don’t have a randomized trial and have to use inferential data,” she noted.
“The take-home points of this trial are that it is a successful international collaboration with a rigorous definition of menopausal status. However, follow-up is still too short to determine the effects of ovarian function suppression on distant tumor recurrence and overall survival,” she said.
“Attention has to be paid to management of toxicity with ovarian function suppression, including endocrine symptoms, hypertension, bone health, and depression,” Dr. Rugo continued.
She said that treatment of premenopausal early-stage breast cancer needs to be individualized, and she proposed the following algorithm: In women with low-risk, node-negative tumors, tamoxifen should be given for at least 5 years. For high-risk patients under the age of 35, ovarian function suppression should be considered due to the marked reduction in breast cancer recurrence. “It is an individualized decision whether we use exemestane or tamoxifen with ovarian function suppression in this group, based on toxicity,” she said. “For intermediate-risk women, ovarian function suppression and endocrine therapy would be reasonable.” ■
Disclosure: Drs. Francis and Ribi reported no potential conflicts of interest. Dr. Arteaga reported research support from Novartis, AstraZeneca, Puma Biotechnology, U3-Daiichi, and OSI-Astellas. Dr. Rugo reported research support to the Regents of the University of California from Novartis, Pfizer, Merck, and Lilly.
References
1. Francis PA, et al: 2014 San Antonio Breast Cancer Symposium. Abstract S3-08. Presented December 12, 2014.
2. Ribi K, et al: 2014 San Antonio Breast Cancer Symposium. Abstract S3-09. Presented December 12, 2014.