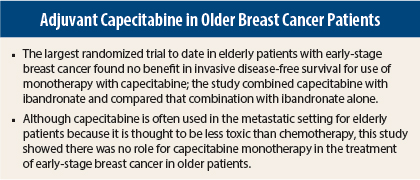
Adjuvant therapy with capecitabine plus ibandronate failed to improve outcomes vs ibandronate alone in elderly patients with moderate-to-high-risk early-stage breast cancer in the ICE study—the largest study to date conducted in elderly women with breast cancer.1
“Capecitabine is frequently used in elderly patients with metastatic disease who cannot tolerate the side effects of conventional chemotherapy. However, if chemotherapy for early breast cancer is indicated due to the biology or the stage of disease, a combination chemotherapy using more than one drug either in sequence or simultaneously is necessary, as the ICE study has shown that monochemotherapy with capecitabine is not working,” said lead author and Chair of the German Breast Group, Gunter von Minckwitz, MD, of the University of Frankfurt, Germany.
“The study showed that one drug is not effective,” he emphasized. “Oncologists should try to give appropriate combination chemotherapy [for stage and aggressiveness] irrespective of age.”
Primary Endpoint
Results of the ICE trial showed no difference between the two treatment arms for the primary endpoint of 3-year invasive disease-free survival: 85.4% in women treated with capecitabine/ibandronate vs 84.3% in the ibandronate-alone arm. The 5-year invasive disease-free survival was 78.8% vs 75%, respectively.
“At 5 years, there was an absolute difference between the arms of 3.8%, but thereafter, the two curves crossed,” Dr. von Minckwitz told listeners.
Closer Look at the ICE Trial
ICE was a prospective, randomized, multicenter trial that enrolled 1,358 patients with node-negative or high-risk node-negative early-stage breast cancer. Women aged 65 or older were randomly assigned 1:1 to receive capecitabine plus ibandronate or ibandronate alone for 2 years of treatment.
Commenting on the study inclusion criteria and treatment arms, Dr. von Minckwitz said: “We excluded patients who were too vulnerable to receive conventional combination chemotherapy and included patients not fit enough for taxane-based chemotherapy. Ibandronate was selected as the backbone for this trial to avoid an untreated control group. We believe these women are at risk for bone-related events anyway, and in 2004 when the trial was started, evidence suggested that ibandronate might prevent breast cancer relapse,” he added.
The mean age was 71 years, and about 25% were aged 75 or older. About 10% had a Charlson comorbidity score of 2, indicating frailty. One-third of patients were on three or more medications for comorbidities. About 14% had triple-negative breast cancer, about 80% had hormone receptor–positive breast cancer, and about 70% were on aromatase inhibitors only.
Interestingly, bone-related events were still frequent in both arms despite the use of a bisphosphonate, he continued. Fractures, surgery, or new osteoporosis (excluding bone metastases) occurred in 25% of the capecitabine/ibandronate group vs 24.7% of the ibandronate-alone arm. About 65% of patients opted to use oral ibandronate, and nearly 35% chose monthly intravenous injections; the mode of administration had no effect on bone-related or other outcomes.
Subgroup analysis mirrored the primary analysis of the trial, with no preferential benefit or deficit for either treatment arm evident in any subgroup.
“In general, despite elderly age and randomization, at the time of the analysis, patients had a favorable 5-year disease-free survival on ibandronate alone. The fact that 75% and 78% were free of disease at 5 years demonstrates that these patients have a lot of life left and should be treated sufficiently, yet they are often undertreated,” Dr. von Minckwitz said.
Combination Chemotherapy
In his view, the result of ICE, together with the results of CALGB 49907 (which showed efficacy for combination chemotherapy vs capecitabine monotherapy), strongly supports the use of combination chemotherapy in elderly women.2 However, toxicity with the combination chemotherapy was twice as high as that with capecitabine (64% vs 33%), which could tip the balance away from combination chemotherapy depending on the patient’s fitness level and disease characteristics.
“The more aggressive the subtype, the more chemotherapy I would use. A patient has to be really unfit before I would not give her chemotherapy,” he said.
In a discussion following his presentation, Dr. von Minckwitz said that when the study was started, there was insufficient evidence of tolerability of combination chemotherapy in elderly women. “Elderly women did not get this treatment when we started the study. Now the data are available and show we can do it,” he said.
Commenting on these results at a press conference, Carlos Arteaga, MD, of Vanderbilt-Ingram Cancer Center in Nashville, and current President of the American Association for Cancer Research, said: “The use of capecitabine in elderly patients with early-stage breast cancer is not supported based on this study. However, that does not exclude the use of other chemotherapy regimens, which may make a difference in outcomes.” ■
Disclosure: This study was funded by Roche and AstraZeneca. Drs. von Minckwitz and Arteaga reported no potential conflicts of interest.
References
1. von Minckwitz G, Reimer T, Potenberg J, et al: The phase III ICE study: Adjuvant ibandronate with or without capecitabine in elderly patients with moderate or high risk early breast cancer. 2014 San Antonio Breast Cancer Symposium. Abstract S3-04. Presented December 11, 2014.
2. Muss HB, Berry DA, Cirrincione CT, et al: Adjuvant chemotherapy in older women with early-stage breast cancer. N Engl J Med 360:2055-2065, 2009.