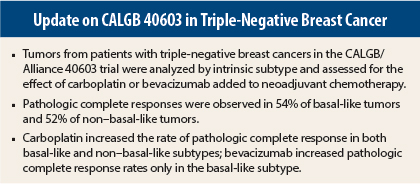
Among women with triple-negative breast cancer, overall, basal-like and non–basal-like tumors were equally likely to demonstrate a pathologic complete response to neoadjuvant chemotherapy, but they responded differently to the addition of carboplatin and bevacizumab (Avastin) to a standard chemotherapy regimen, according to an analysis of CALGB/Alliance 40603 presented at the 2014 San Antonio Breast Cancer Symposium.1
“The magnitude of pathologic complete response benefit with carboplatin was consistent across subtypes, while a basal-like pattern was predictive of a greater pathologic complete response increment with bevacizumab,” said
William Sikov, MD, of Women and Infants Hospital and the Alpert Medical School of Brown University, Providence, Rhode Island.
Although carboplatin increased pathologic complete response rates equally for women with basal-like and non–basal-like tumors, the addition of bevacizumab contributed benefit only among women with basal-like tumors, and the drug actually diminished pathologic complete responses in women with non–basal-like cancers, he said.
CALGB 40603 Details
The randomized phase II trial included 443 patients with stage II-III triple-negative breast cancer who underwent neoadjuvant chemotherapy. The study evaluated the benefit of adding carboplatin (AUC [area under the curve] 6) or bevacizumab (10 mg/kg) to a standard neoadjuvant regimen of paclitaxel (80 mg/m2 weekly) followed by dose-dense doxorubicin and cyclophosphamide.
At the 2013 San Antonio Breast Cancer Symposium, Dr. Sikov and colleagues reported that either agent increased pathologic complete response rates.2 In this analysis, the investigators drilled deeper for a closer examination of 360 tumor samples by intrinsic subtype. They classified the tumors as basal-like (n = 314)—which accounted for 87% of the samples and tends to carry a worse prognosis—or non–basal-like (n = 46). Non–basal-like tumors were a mix of subtypes, including HER2-enriched, normal-like, claudin-low, and luminal A.
The overall pathologic complete response rate in these subtyped samples did not differ between basal-like (54%) and non–basal-like (52%) tumors, but some treatment interactions were noted.
In patients in the basal-like cohort randomized to receive carboplatin or no carboplatin, pathologic complete response in the breast was achieved by 61% of the carboplatin arm vs 47% in the standard chemotherapy arm (odds ratio = 1.76, P = .014). The findings were similar for non–basal-like tumors, where pathologic complete responses were achieved by 58% and 45%, respectively (odds ratio = 1.67, P = .55).
“The interesting thing was that, for the addition of carboplatin, the benefit was equivalent in basal-like and non–basal-like cancers. This doesn’t mean that carboplatin was of no benefit in the basal-like subtype, only that there was no amplification of benefit vs the non–basal-like subtype,” he explained.
In contrast, subtype was important for the achievement of pathologic complete response in the bevacizumab cohorts. The benefit with bevacizumab was significantly greater in the basal-like subtype, more than doubling the odds of achieving a pathologic complete response. In basal-like patients, pathologic complete response rates were 64% with bevacizumab and 45% without (odds ratio = 2.15, P = .0009), but for the other subtypes, the rates were 43% and 60%, respectively (odds ratio = 0.50, P = .25), indicating a trend toward worse responses when bevacizumab was added.
CALGB 40603 also showed that higher levels of expression of any of five immune signatures, reflecting an increase in tumor-infiltrating lymphocytes, were associated with higher pathologic complete response rates. Expression of high proliferation, low estrogen expression, or high TP53-mutation signatures, in particular, was predictive of higher pathologic complete response rates overall and greater pathologic complete response benefit from the addition of bevacizumab, Dr. Sikov also reported.
“None of these signatures was predictive of greater pathologic complete response benefit for carboplatin in all patients or in the basal-like subset,” he added.
Not Likely to Change Practice
“Although these are interesting observations, I don’t think our data will change clinical practice,” Dr. Sikov acknowledged. Interest in using bevacizumab in early-stage triple-negative disease has diminished following disappointing results from several phase III studies, he said. Regarding the role of carboplatin in the neoadjuvant setting for triple-negative disease, he said, “The jury is still out.”
Dr. Sikov said that these data will probably reinforce the way clinicians already view the use of carboplatin in early-stage triple-negative disease. Some clinicians feel that the 14% absolute increase in pathologic complete response rates with the addition of carboplatin is encouraging and could benefit their high-risk triple-negative patients, especially since its use is associated with relatively modest increases in hematologic toxicities, and the drug is familiar and inexpensive.
Other clinicians may think the absolute increase in the pathologic complete response rate is not high enough to convince them of the benefit of adding carboplatin, will point to the increase of toxicity and the lack of long-term outcomes, and will conclude that the available data does not support the use of carboplatin outside of a clinical trial, he said.
“A risk/benefit assessment must be done with the patient and clinician together,” he concluded.
In an interview, John Cole, MD, Head of Medical Oncology at the Ochsner Clinic Foundation in New Orleans, commented that he does not yet use carboplatin in the neoadjuvant treatment of triple-negative cancers, and before he does, he would like to see a subset of patients likely to benefit.
“There are no clear, compelling data yet on the use of carboplatin at this point. We are trying to find a way to enrich the population of patients who might benefit from this (and bevacizumab),” he said.
He was curious about the high rate (87%) of cancers that were subtyped as basal-like, since this is much higher than observed in other studies. “It makes you wonder a bit about patient selection,” Dr. Cole continued. He said he would also like to know what percentage were BRCA mutation–positive and what their outcomes were. “This is an important question, because this might be the group getting the most bang, while others are not,” he said. ■
Disclosure: Drs. Sikov and Cole reported no potential conflicts of interest.
References
1. Sikov WM, et al: 2014 San Antonio Breast Cancer Symposium. Abstract S4-05. Presented December 11, 2014.
2. Sikov WM, et al: 2013 San Antonio Breast Cancer Symposium. Abstract S5-01. Presented December 13, 2013.