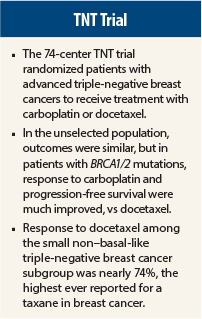
The TNT trial, presented at the 2014 San Antonio Breast Cancer Symposium, provided no evidence that unselected advanced triple-negative breast cancer patients are more likely to respond to carboplatin than to docetaxel.1 However, patients with BRCA1/2 mutations do have a greater response and a longer progression-free survival with carboplatin, according to Andrew Tutt, MB, ChB, PhD, MRCP, FRCR, of Kings College and Institute of Cancer Research London.
“The TNT trial supports BRCA1/2 genotyping to inform therapy choice in metastatic triple-negative breast cancer and familial breast cancer,” Dr. Tutt said.
TNT Details
Subgroups within triple-negative breast cancers appear to share impaired DNA repair mechanisms—in particular, homologous recombination repair deficiency (HRD)—with BRCA1/2 germline mutation–positive patients. This impairment is thought to confer sensitivity to platinum agents. The TNT trial tested this hypothesis in women with recurrent locally advanced or metastatic BRCA-positive tumors or triple-negative breast cancer.
According to Dr. Tutt, TNT is the first study to directly compare single-agent platinum chemotherapy with the mechanistically distinct taxanes in these populations. The study included 376 patients (91% with metastatic disease) from 74 centers in the United Kingdom. A total of 43 mutations were identified. A BRCA1/2 germline mutation was noted for 9% of the carboplatin arm and 6.4% of the docetaxel arm.
Patients were randomly assigned to receive carboplatin (area under the curve of 6 every 3 weeks) or docetaxel (100 mg/m2 every 3 weeks) for 6 to 8 cycles or until disease progression, with crossover possible on disease progression. The primary endpoint was intent-to-treat objective response rate to cycle 6. TNT aimed to detect a 15% improvement in response with carboplatin compared with docetaxel.
Unselected Population
After a median follow-up of 11 months, objective responses were observed in 59 of 188 patients (31.4%) in the carboplatin arm and 67 of 188 patients (35.6%) in the docetaxel arm, for an absolute difference of –4.2% (carboplatin response rate minus docetaxel response rate; 95% confidence interval [CI] = –13.7% to 5.3%), which was not statistically significant (P = .44). Similarly, after crossover (n = 182), the response rates were 2.8% higher for the docetaxel cohort crossing over to receive carboplatin (95% CI = –9.6% to 15.2%), but again, this was not statistically significant (P = .73).
The median progression-free survival was 3.1 months (95% CI = 2.5 to 4.2) in the carboplatin arm and 4.5 months (95% CI = 4.1 to 5.2) in the docetaxel arm (P = .29). The median overall survival was 12.4 months (95% CI = 10.4 to 15.3) and 12.3 months (95% CI = 10.5 to 13.6) respectively (P = .31), Dr. Tutt reported.
BRCA1/2-Positive Population
Among the 43 BRCA-positive patients, however, a difference emerged between the regimens. The objective response rate was 68% with carboplatin and 33% with docetaxel, a 34.7% absolute difference (95% CI = 6.3% to 63.1%), which was statistically significant (P = .03). In contrast, for the 273 BRCA-negative patients, response rates were not significantly different at 28.1% and 36.6% (absolute difference = –8.5%, 95% CI = –19.6% to 2.6%), respectively (P = 0.16).
“Carboplatin demonstrated significantly increased activity vs docetaxel in BRCA carriers, and there was a positive test for the interaction between the randomization arm and BRCA1/2 status (P = .01),” Dr. Tutt noted.
This finding was obvious by the difference observed in the carboplatin arm according to BRCA status: BRCA-positive patients had a median progression-free survival of 6.8 months (95% CI = 4.4 to 8.1), compared with 3.1 months (95% CI = 2.4 to 4.2) in patients with nonmutated BRCA receiving carboplatin. The differences were not seen with docetaxel.
“In the metastatic setting, it’s important to know the BRCA status of patients and for a platinum to be considered among their treatment options,” Dr. Tutt said.
HRD Score Findings
The HRD score was available for 195 patients, with 81 patients classified as HRD “high” (≥ 42) and 114 as HRD “low” (< 42). (For 25 patients, the test failed.) Dr. Tutt explained that this score was the mean of three analyses by Myriad Genetics and is now the company’s published cut-point.
“The dichotomized HRD score did not select for sensitivity to carboplatin over docetaxel when conducted on the primary tumor DNA,” Dr. Tutt indicated. “BRCA1/2-mutant tumors, as expected, had high HRD scores.”
Response rates were 38.2% in HRD-high patients receiving carboplatin and 42.6% for those receiving docetaxel (absolute difference = –4.4%, 95% CI = –26.0% to 17.2%, P = .82). Among the HRD-low patients, response rates were 29.2% to carboplatin and 34.7% to docetaxel (absolute difference = –5.4%, 95% CI = –22.7% to 11.9%, P = .55).
The investigators proposed that nonmutated HRD-high cancers may more frequently reverse the homologous repair defect in metastases than mutated tumors.
“We feel that further development of homologous recombination defect assays for BRCA status in non-BRCA1/2 tumors is required, especially in the metastatic setting,” Dr. Tutt suggested.
The investigators also observed similar performance between carboplatin and docetaxel in both core basal-like (by central immunohistochemistry) and PAM50-based Prosigna assay basal-like subgroups. However, in the nonbasal subtype by the PAM50-based Prosigna assay, response to docetaxel was much greater than to carboplatin: 73.7% vs 16.7% with carboplatin (absolute difference = –55.5%, 95% CI = –82.4% to –28.6%, P = .01) The test for interaction was significant (P = .01).
“Although the TNT trial gave no evidence to support superior activity of carboplatin over docetaxel in unselected triple-negative breast cancer patients, the results for germline BRCA-positive patients supported their greater sensitivity to carboplatin,” Dr. Tutt concluded. ■
Disclosure: Dr. Tutt reported no potential conflicts of interest.
Reference
1. Tutt A, et al: The TNT trial. 2014 San Antonio Breast Cancer Symposium. Abstract S3-01. Presented December 11, 2014.