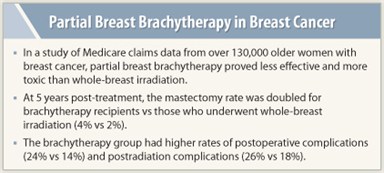
Partial breast brachytherapy is less effective and more toxic than whole-breast irradiation when used after lumpectomy, suggests an analysis of Medicare claims data.
 In the 2000–2007 study of more than 130,000 older women with breast cancer—the largest of its kind to date—the rate of mastectomy in the 5 years after treatment (a surrogate of treatment effectiveness) was doubled for those who received brachytherapy compared with those who received whole-breast irradiation, although still very low (4% vs 2%).
In the 2000–2007 study of more than 130,000 older women with breast cancer—the largest of its kind to date—the rate of mastectomy in the 5 years after treatment (a surrogate of treatment effectiveness) was doubled for those who received brachytherapy compared with those who received whole-breast irradiation, although still very low (4% vs 2%).
The brachytherapy group also had higher rates of postoperative complications (24% vs 14%) and postradiation complications (26% vs 18%), coinvestigator Benjamin D. Smith, MD, reported at the 2011 San Antonio Breast Cancer Symposium.1
Collectively, the results call into question the role of brachytherapy, which has advantages in terms of treatment duration and potentially compliance, but is increasingly being used despite a lack of long-term randomized data.
Study Limitations
Dr. Smith acknowledged several study limitations, such as the inability to determine the reason for mastectomy (although most were likely done for recurrence) and the role of unmeasured confounders. “There are other important outcomes that may not generate claims or a medical encounter in the treatment of breast cancer,” he added. “One of these outcomes would be the aesthetic outcome of the breast after breast-conserving therapy.”
Whether the results still apply today is unclear, according to Dr. Smith, who is an Assistant Professor in the Department of Radiation Oncology at The University of Texas MD Anderson Cancer Center, Houston. “We don’t know the extent to which there is a learning curve with brachytherapy or the extent to which newer brachytherapy techniques may or may not improve outcomes,” he explained.
Also unknown is whether the findings apply to younger women. “We have an ongoing intergroup study evaluating partial breast compared to whole-breast irradiation in women under the age of 50, and I think such patients interested in partial breast irradiation are ideally suited for enrollment on that trial rather than off-protocol treatment,” he said.
Long-term Data to Come

 “This is an interesting study, though it is only looking at one way of giving APBI [accelerated partial breast irradiation]—brachytherapy,” Lori J. Pierce, MD, Professor of Radiation Oncology at the University of Michigan in Ann Arbor, commented in an interview. “And while there are limitations in how best to interpret the data, it is a large study, and the results should be considered while we await results from randomized trials of partial-breast vs whole-breast radiotherapy.”
“This is an interesting study, though it is only looking at one way of giving APBI [accelerated partial breast irradiation]—brachytherapy,” Lori J. Pierce, MD, Professor of Radiation Oncology at the University of Michigan in Ann Arbor, commented in an interview. “And while there are limitations in how best to interpret the data, it is a large study, and the results should be considered while we await results from randomized trials of partial-breast vs whole-breast radiotherapy.”
Julie Gralow, MD, Director of Breast Oncology at the University of Washington, cautioned that the field has other examples where practice has gotten ahead of the research. “We’ve jumped into some things in breast cancer where we start rolling down the road and we can’t pull back and wait for randomized clinical trial data, and one of them has been partial breast irradiation,” she commented in an interview.
Importantly, the study did not assess the costs of brachytherapy, which is billed to Medicare at a higher rate, according to Dr. Gralow.
Study Details
 Investigators analyzed Medicare data, identifying women aged 67 years or older who had an early invasive breast cancer diagnosis between 2000 and 2007 and underwent lumpectomy followed by some type of radiation therapy. Using claims data, they compared outcomes between 123,244 women who received whole-breast irradiation and 7,291 who received brachytherapy (about three-fourths of whom had single-entry catheter–based brachytherapy, codes suggested).
Investigators analyzed Medicare data, identifying women aged 67 years or older who had an early invasive breast cancer diagnosis between 2000 and 2007 and underwent lumpectomy followed by some type of radiation therapy. Using claims data, they compared outcomes between 123,244 women who received whole-breast irradiation and 7,291 who received brachytherapy (about three-fourths of whom had single-entry catheter–based brachytherapy, codes suggested).
The patients were 75 years old, on average. About 76% had some type of axillary surgery. Only a minority received chemotherapy (14%) and had axillary node involvement (12%). Their median follow-up was 3.8 years.
Analysis of temporal trends showed that use of brachytherapy increased significantly and sharply over time. It was used in less than 1% of patients overall in 2000 but in 13% by 2007.
Patients in the brachytherapy group had a significant doubling of the rate of mastectomy at 5 years relative to their counterparts in the whole-breast irradiation group (4% vs 2%). The difference persisted in multivariate analysis (HR = 2.22) and was similar regardless of the broad type of brachytherapy.
“It’s very plausible to think that the majority of these mastectomies were done for recurrence,” Dr. Smith commented. “The most intuitive explanation is that some patients who are treated with brachytherapy had residual tumor cells in the breast that were outside the confines of the target volume for brachytherapy.”
Other Key Results
The difference between groups was greater in patients who had had axillary lymph node involvement (HR = 4.69) than in those who had not (HR = 2.06). Overall survival, another measure of effectiveness, did not differ between groups.
Patients had significantly higher 1-year rates of postoperative complications after brachytherapy than after whole-breast irradiation, in terms of both infections and other complications.
The brachytherapy group also had significantly higher 5-year cumulative rates of certain postradiation complications. The whole-breast irradiation group had a significantly higher rate of radiation. ■
Disclosure: Dr. Smith has received research funding from Varian Medical Systems, but that funding was not used for any part of this study, which was funded by a grant from the Department of Defense and by institutional sources. Drs. Gralow and Pierce reported no potential conflicts of interest.
Reference
1. Smith GL, Xu Y, Buchholz TA, et al: Partial breast brachytherapy is associated with inferior effectiveness and increased toxicity compared with whole breast irradiation in older patients. San Antonio Breast Cancer Symposium. Abstract S2-1. Presented December 7, 2011.

