The Russian Federation is the largest country in the world, extending from Eastern Europe to Northern Asia and the Pacific Ocean. The population of more than 140 million people is unevenly distributed across the country.1 As a result, Russia has high spatial inequality in terms of accessibility of primary and specialized medical care. In addition, Russia faces an aging population, with an increase in the old-age dependency ratio (ie, the number of older people at an age when they are generally economically inactive compared with the number of people of working age) from 18% to 23.5% over the past 20 years.1 The general demographic profile of Russia is summarized in Table 1.

Cancer Profile in Russia
In Russia, national cancer statistics are obtained from regional population–based cancer registries and civil registries, with the former providing data on incidence and the latter, on mortality.2 In 1953, Russia (then part of the Union of Soviet Socialist Republics) introduced mandatory cancer registration. However, it was only in the late 1990s that regional population–based cancer registries, which collect and store individual-level data, were fully established on a national scale. As a result, national cancer incidence data are available from 1993, whereas cancer-related mortality can be traced back to the early 1960s.
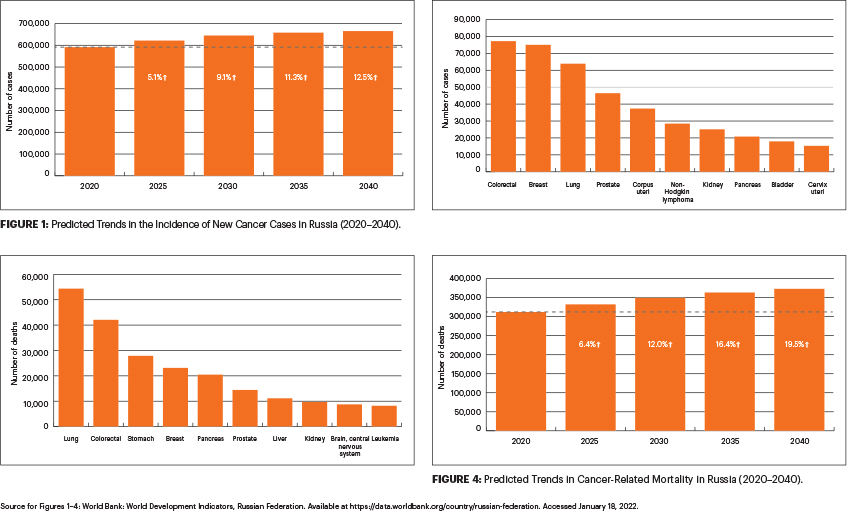
The increasing cancer incidence trends in Russia reflect the growing burden of risk factors and, more recently, the enhanced availability of diagnostic services. In 2019, according to the National Cancer Report, there were more than 291,000 new cancer cases in men and 348,000 in women. The predicted trends show that, without intervention, cancer incidence in Russia is expected to rise almost 13% in the next few decades (Figure 1).
The latest available data show that, in 2020, the most common cancer by incidence in Russia was colorectal cancer, followed by breast cancer and lung cancer (Figure 2). Incidence rates of colorectal cancer have consistently increased over the past 3 decades (from 16.9 to 24.3 per 100,000 women and 22.7 to 35.3 per 100,000 men between 1993 and 2019), reflecting changes in the prevalence of risk factors, an aging population, and the availability of diagnostic services in Russia. On the other hand, the incidence rate of gastric cancer has declined for both men and women due to a combination of improved sanitary conditions and a possible decrease in the prevalence of Helicobacter pylori infection.3
Prostate cancer incidence rates increased from 9.7 in 1993 to 44.2 in 2019 per 100,000 men. In the corresponding period, breast cancer incidence rates in women also increased from 33.1 to 54.2 per 100,000. Although this is similar to many other developed countries, it is still twice as low in Russia than in other countries with established screening programs.4
Despite the initial overall modest levels of cervical cancer burden, the incidence rates have uniformly increased over the past 3 decades from 10.6 to 15.6 per 100,000. Cervical cancer is currently one of the most common cancers diagnosed in women younger than age 45. In contrast to most European countries, the incidence of lung cancer in women remains low, possibly reflecting the low prevalence of tobacco smoking.5
Cancer remains one of the leading causes of death in Russia, second only to deaths from cardiovascular diseases. In 2019, more than 158,000 men and 136,000 women died of cancer. Cancer-related mortality peaked in Russia in 1993 to 1994, after which there has been a steady decline in deaths related to cancer.
Lung cancer remains the leading cause of cancer-related mortality in Russia, with more than 54,000 deaths in 2020 (Figure 3). Although stomach cancer was the second most common cause of cancer-related deaths in the later part of the 20th century, it has now been replaced by colorectal cancer. Despite high incidence rates, the mortality from prostate cancer remains low. Breast cancer is currently a leading cause of cancer-related death in Russian women. However, we have noted a recent decline in breast cancer–related mortality, which could be attributed to a combination of better treatment options and greater availability of adjuvant therapy. In contrast, the cervical cancer–related mortality has been relatively stable, hiding the underlying risk factors.4
Predicted trends show that the number of cancer-related deaths is expected to rise 19.5% over the next 2 decades, from around 312,000 deaths in 2020 to 373,000 deaths in 2040 (Figure 4). An aging population may be the main reason behind this rise in the absolute number of deaths, despite a decrease in overall cancer-related mortality rates.
The loss of economic productivity due to premature cancer-related mortality in Russia is substantial and amounts to $8 billion per year.6 The greatest loss in economic productivity is noted in women with breast cancer and in men with lung cancer. Although breast and lung cancers account for the greatest loss, the incremental rise in the loss of economic productivity is highest in patients with human papillomavirus (HPV)-related cancers. This emphasizes the importance of HPV vaccination, which is yet to be implemented on a national scale in Russia.
Cancer Control Initiatives
A national health checkup, or “dispensarization,” program was initiated in 2013 and includes several diagnostic tests for cancer screening (eg, mammography, cervical cytology, fecal occult blood test, prostate-specific antigen test). These tests are performed in nononcologic health-care clinics. Despite the lack of quality control, recent period changes in cancer incidence can likely be attributed to this program. The effect on cancer mortality has not yet been apparent and should be studied using individual-level data.
Russia has universal health coverage. All citizens have an option of free treatment in state-run medical facilities through social health insurance funded by mandatory employer contributions. Russia faces problems related to the implementation of high-tech medical care and low wages for medical personnel. Medical resources are traditionally unevenly distributed between primary health state clinics and centers of excellence.
Apart from unhealthy behavior, the reasons for less-than-optimal population health may lie in the health-care system’s suboptimal financing and inefficient resource allocation. The total health-care expenditure was 5.3% of the gross domestic product,1 which is much less than the Organisation for Economic Co-operation and Development average. The share of voluntary health insurance is minimal, and private health-care expenditures are primarily out-of-pocket.

Barriers to Cancer Care
In Russia, “oncology” is designated as a specialty that includes physicians practicing medical, surgical, and radiation oncology. Training typically lasts 2 years immediately following medical school, with an additional 4-month course recommended for a radiation oncologist. In contrast, countries with a Human Development Index—a summary measure of average achievement in key dimensions of human development: a long and healthy life, being knowledgeable, and having a satisfactory standard of living—require 6 to 9 years of training, depending on the specialty.7
There is also no board certification administered by a professional society that establishes quality standards for the specialties. At the same time, the shortage of oncologists was estimated at about 2,000 physicians. As a result, novel educational initiatives such as the Higher School of Oncology are emerging.8,9 The aims of these initiatives are to introduce the current platforms of modern postgraduate training into the Russian health-care system.
Cancer care in Russia is traditionally concentrated in regional tertiary care oncology centers known as “dispensaries.” Large tertiary care oncology centers admit patients with an established diagnosis of cancer following workup at other centers. Following referral to the tertiary care center, the oncologist completes tumor staging and verification and then presents the case to the multidisciplinary team, which, by practice, makes all critical treatment decisions.
Several federal cancer centers provide the full spectrum of modern cancer care. Many patients travel great distances to receive appropriate cancer care, which partially explains why most cancer surgeries, chemotherapy, and radiation treatments require a hospital stay. An outpatient oncologist, who usually does not participate in the primary treatment, provides the follow-up care in a stand-alone public clinic upon the patient’s discharge from the tertiary care cancer center. In case of a relapse, the oncologist refers the patient back to the tertiary care cancer center for treatment planning at a multidisciplinary team meeting. Whether this general workflow offers high-quality and timely cancer care has yet to be determined.
Investigator-initiated research is rare in Russia. A few original breast cancer clinical trials and a recent colorectal cancer surgery trial are worth mentioning.10,11 Observational studies sometimes make it into international peer-reviewed journals, but most researchers publish in Russian journals. Lack of training in modern epidemiology and biostatistics limits the opportunities to design and conduct population-based studies. The deficiencies in research also contribute to a low adherence to evidence-based medicine in oncology. However, the recent trend to computerize Russian health care may provide valuable real-world, individual-level data to test a wide range of research hypotheses.
Further Efforts to Improve Cancer Care
The National Cancer Control Plan for 2019 to 2024 calls for a new network of outpatient cancer diagnostic and treatment facilities.12 The initiative aims to shorten the time frames for workup, tackle spatial inequality in terms of the accessibility of cancer care, and provide management and follow-up for patients who do not require hospitalization. It is envisaged that all these initiatives, over a period of time, will improve the cancer care landscape in Russia.

Anton Barchuk, MD, PhD

Yulia Raskina, PhD

Rustam Tursun-Zade

Hope Craig, MSPH

Chandrakanth Are, MBBS, MBA, FSSO, FRCS, FACS
Vadim Gushchin, MD, FACS, FSSO
Dr. Barchuk is Associate Professor, European University at St. Petersburg, and Chief Executive Officer, Association of Oncologists or Northwestern Federal District, St. Petersburg. Dr. Raskina is Assistant Professor, European University at St. Petersburg. Mr. Tursun-Zade is a research scientist at the European University at St. Petersburg. Ms. Craig is Research Support Specialist at Cornell University, Ithaca, New York. Dr. Are is the Jerald L & Carolynn J. Varner Professor of Surgical Oncology & Global Health; Associate Dean for Graduate Medical Education; and Vice Chair of Education Department of Surgery, University of Nebraska Medical Center, Omaha. Dr. Gushchin is Director of Gastrointestinal Oncology at Mercy Medical Center, Baltimore.
DISCLOSURE: Dr. Barchuk has served as a consultant or advisor to Biocad and MSD. Dr. Raskina, Mr. Tursun-Zade, Ms. Craig, and Dr. Gushchin reported no conflicts of interest. Dr. Are is a board member with Global Laparoscopy Solutions; has received research funding from Pfizer; and has a patent with the University of Nebraska Medical Center for a laparoscopy instrument.
REFERENCES
1. World Bank: World Development Indicators, Russian Federation. Available at https://data.worldbank.org/country/russian-federation. Accessed January 18, 2022.
2. Barchuk A, Belyaev A, Gretsova O, et al: History and current status of cancer registration in Russia. Cancer Epidemiol 73:101963, 2021.
3. Tkachenko MA, Zhannat NZ, Erman LV, et al: Dramatic changes in the prevalence of Helicobacter pylori infection during childhood: A 10-year follow-up study in Russia. J Pediatr Gastroenterol Nutr 45:428-432, 2007.
4. Barchuk A, Bespalov A, Huhtala H, et al: Breast and cervical cancer incidence and mortality trends in Russia 1980–2013. Cancer Epidemiol 55:73-80, 2018.
5. Ng M, Freeman MK, Fleming TD, et al: Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA 311:183-192, 2014.
6. International Agency for Research on Cancer, World Health Organization: Cancer Today/Population Fact Sheets: Russia, Globocan 2020. Available at https://gco.iarc.fr/today/home. Accessed January 18, 2022.
7. Barchuk A, Bespalov A, Huhtala H, et al: Productivity losses associated with premature mortality due to cancer in Russia: A population-wide study covering 2001–2030. Scand J Public Health 47:482-491, 2019.
8. Are C, Caniglia A, Malik M, et al: Variations in training of surgical oncologists: Proposal for a global curriculum. Eur J Surg Oncol 42:767-778, 2016.
9. Baron E, Sittig M, Kotov M, et al: Educational collaboration between Russian-born US physicians andRussian oncology trainees in evidence-based medicine: The higher school of oncology. JCO Glob Oncol 7:353-360, 2021.
10. Semiglazov VF, Topuzov EE, Bavli JL, et al: Primary (neoadjuvant) chemotherapy and radiotherapy compared with primary radiotherapy alone in stage IIb-IIIa breast cancer. Ann Oncol 5:591-595, 1994.
11. Karachun A, Panaiotti L, Chernikovskiy I, et al: Short-term outcomes of a multicentre randomized clinical trial comparing D2 versus D3 lymph node dissection for colonic cancer (COLD trial). Br J Surg 107:499-508, 2020.
12. Petrovsky A, Tjulandin S, Tryakin A, et al: Creation and development of the National Cancer Control Plan in Russia. J Clin Oncol 37(suppl 15):10524, 2019.

