In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
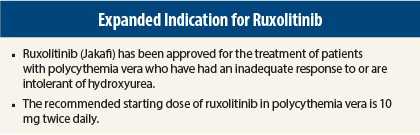
On December 4, 2014, ruxolitinib (Jakafi) was approved for the treatment of patients with polycythemia vera who have had an inadequate response to or are intolerant of hydroxyurea.1,2
Ruxolitinib was initially approved in November 2011 for treatment of patients with intermediate-risk or high-risk myelofibrosis.
Supporting Trial
Approval was based on findings in an open-label phase III trial in which 222 patients with polycythemia vera resistant to hydroxyurea or who could not tolerate hydroxyurea were randomly assigned to receive oral ruxolitinib at a starting dose of 10 mg twice daily (n = 110) or best available care (n = 112). The ruxolitinib dose could be increased to 25 mg twice daily. Patients had to require phlebotomy, had to have splenomegaly, and had to have hematocrit control between 40% and 45% prior to randomization.
Patients ranged in age from 33 to 90 years (30% > 65 years), and 66% were male. Best available therapy included hydroxyurea (60%), interferon/pegylated interferon (12%), anagrelide (7%), pipobroman (Vercyte) (2%), lenalidomide (Revlimid)/thalidomide (Thalomid) (5%), and observation (15%).
Ruxolitinib was superior to best available therapy in achieving the composite endpoint of durable hematocrit control (absence of phlebotomy eligibility beginning at week 8 and maintained thereafter) and spleen volume reduction (≥ 35% reduction) at week 32 (21% vs 1%, P < .0001) and at week 48 (19% vs 1%, P < .0001). Complete hematologic remission at week 32 was achieved in 24% vs 9% (P = .0034). At week 32, 60% vs 20% of patients had hematocrit control and 38% vs < 1% had spleen volume reduction ≥ 35%.
How It Works
Ruxolitinib inhibits Janus kinases (JAKs) JAK1 and JAK2, which mediate signaling of cytokines and growth factors involved in hematopoiesis and immune function. JAK signaling involves recruitment of STATs to cytokine receptors and activation and localization of STATs to the nucleus, leading to modulation of gene expression. Polycythemia vera is associated with dysregulated JAK1 and JAK2 signaling. In a mouse model of JAK2-mutant myeloproliferative neoplasms, ruxolitinib prevented splenomegaly, preferentially decreased JAK2 mutant cells in the spleen, and decreased circulating inflammatory cytokines.
How It Is Given
The recommended starting dose of ruxolitinib in polycythemia vera is 10 mg twice daily. The starting dose is 5 mg twice daily in patients taking strong CYP3A4 inhibitors (eg, ritonavir, idinavir, clarithromycin, ketoconazole, itraconazole), those with moderate to severe renal impairment, and those with hepatic impairment.
Doses may be titrated based on safety and efficacy evaluations. Complete blood counts and platelet counts must be performed before starting therapy, every 2 to 4 weeks until doses are stabilized, and then as clinically indicated. Serious infections should have resolved before ruxolitinib treatment is started.
Detailed recommendations for dose modifications and interruptions based on hemoglobin, platelet count, and neutrophil count are provided in product labeling. In patients with insufficient response who have adequate platelet, hemoglobin, and neutrophil counts, doses may be increased in increments of 5 mg twice daily to a maximum of 25 mg twice daily.
Doses should not be increased during the first 4 weeks of therapy and not more frequently than every 2 weeks. In patients restarting ruxolitinib after treatment interruption, except interruption due to phlebotomy-associated anemia, doses may be increased to a maximum total daily dose not exceeding 5 mg less than the dose resulting in interruption.
Safety Profile
The most common hematologic adverse events of any grade in the ruxolitinib group in the phase III trial were anemia (72%, including < 1% grade 3 and < 1% grade 4, vs 58% in the control group, with no grade 3 or 4 events) and thrombocytopenia (27%, including 5% grade 3 and < 1% grade 4, vs 24%, including 3% grade 3 and < 1% grade 4). The most common nonhematologic adverse events of any grade were headache (16% vs 19%), abdominal pain (15% vs 15%), diarrhea (15% vs 7%), dizziness (15% vs 13%), and fatigue (15% vs 15%).
The only grade 3 or 4 adverse event occurring in > 1% of ruxolitinib patients was dyspnea (3% vs 0%). Ruxolitinib treatment was discontinued due to adverse events in 4% of patients.
Ruxolitinib carries warnings/precautions for thrombocytopenia, anemia, and neutropenia; infection; symptom exacerbation following treatment interruption or discontinuation; and risk of nonmelanoma skin cancer.
Report Adverse Events
Health-care professionals should report all serious adverse events suspected to be associated with the use of any medicine or device to FDA’s MedWatch Reporting System by completing a form online at www.fda.gov/medwatch/report.htm, by faxing (800-FDA-0178), by mailing the postage-paid address form provided online, or by telephone (800-FDA-1088). ■
References
1. U.S. Food and Drug Administration: Ruxolitinib. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm425732.htm. Accessed December 23, 2014.
2. Jakafi® (ruxolitinib) tablets prescribing information, Incyte Corporation, December 2014. Available at www.incyte.com/sites/default/files/Jakafi_PI.pdf?time=20141215104415. Accessed December 23, 2014.