For the treatment of high-risk, treatment-naive myelodysplastic syndromes (MDS), the regimen of venetoclax plus azacitidine led to high response rates, durable responses, and encouraging overall survival, in a phase Ib study reported at the 2023 American Society of Hematology (ASH) Annual Meeting & Exposition.1
“The venetoclax plus azacitidine combination had favorable responses of complete remission [30%] plus marrow complete remission [50%] in more than 80% of patients and overall hematologic improvement in nearly 50%. Duration of complete response was more than 16 months, and median overall survival was 26 months,” according to Jacqueline S. Garcia, MD, of Dana-Farber Cancer Institute, Boston. “Of note, with these two drugs, the disease-progression rate was only 1.9%, meaning most patients who initiated therapy on study did achieve some sort of benefit.”

With [venetoclax and azacitidine], the disease-progression rate was only 1.9%, meaning most patients who initiated therapy on study did achieve some sort of benefit.— Jacqueline S. Garcia, MD
Tweet this quote
Venetoclax, a BCL2 inhibitor, and azacitidine, a hypomethylating agent, have synergy, and this combination is being used in acute myeloid leukemia (AML). Since MDS is closely associated with—and often evolves into—AML, researchers have begun to evaluate the combination in MDS.
About M15-531
The 124 patients in the phase Ib M15-531 study had de novo high-risk MDS, blasts less than 20% at baseline, no prior treatment for MDS, no prior transplant, and no history of active malignancy within the past 2 years. Of the 124 patients, 107 received venetoclax at the recommended phase II dose of 400 mg orally daily on days 1 to 14 of each 28-day cycle; the remainder received 100 mg to 400 mg of venetoclax. Patients also received azacitidine at 75 mg/m2 on days 1 to 7 or days 1 to 5, 8, and 9, until disease progression. The primary endpoint of the presented analysis from the recommended phase II dose cohort was complete remission according to International Working Group (IWG) 2006 criteria.
“This was a high-risk population, with more than 85% having mutations that generally portend a poor prognosis,” Dr. Garcia said. The majority of patients (60%) had blasts > 10%, and more than 90% had > 5% blasts; median baseline blast count was very high in 59% of patients, and 64% had intermediate-to-very-poor cytogenetic risk. The most common mutations were ASXL1 (35%), TP53 (24%), SRSF2 (23%), and RUNX1 (21%).
Key Outcomes
At a median follow-up of 32 months, for the 107 patients receiving the recommended dose, the modified overall response rate (defined per protocol as complete remission plus marrow complete remission plus partial remission according to IWG 2006 criteria) was 80.4%; the rate of complete remission was 29.9% (n = 32/107); the rate of marrow complete remission was 50.5% (n = 54/107); and the rate of marrow complete remission plus hematologic improvement was 37.0% (n = 20/54). Stable disease was observed in 10.3% of patients; 7.5% were not evaluable; and 1.9% had progressive disease as their best response.
“The duration of complete remission was long and impressive,” Dr. Garcia commented. The median number of treatment cycles with the regimen was four; however, for those who did not proceed to transplant, the median number of cycles was seven. The median time to complete remission was 2.7 months, and the median duration of complete remission was 16.6 months. Once achieved, complete remission lasted a median of 12 months for 60.2% of patients and 24 months for 42.6%. Approximately 12% transformed from MDS to AML, and this occurred at a median of about 6 months for these patients, she reported.
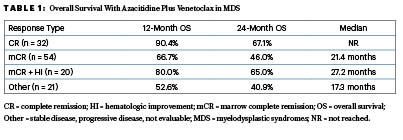
Overall Survival by Response
The median overall survival was 26 months, with an overall survival rate of 71.2% at 12 months and 51.3% at 24 months. “Responses did portend an improvement in survival,” said Dr. Garcia, who reported overall survival data according to response (Table 1) for all dose cohorts.
Importantly, the median overall survival for patients that achieved complete remission has not yet been reached and 27.2 months for those with marrow complete remission plus hematologic improvement. The phase III randomized, double-blinded trial (VERONA) with azacitidine plus placebo or venetoclax in untreated patients with higher-risk MDS is eagerly awaited; the primary endpoint is overall survival.
Transfusions and Subsequent Treatment
Approximately 58% of the patients received subsequent treatment, which for 41% included allogeneic stem cell transplantation. The median time to the next treatment from the first study dose was 6.8 months, and it was 13.4 months when transplantation was excluded. The median time to transplant was 4.8 months. Other treatments after the study included single-agent azacitidine in 12.1%, decitabine in 4.7%, and venetoclax in 2.8%.

This is not a randomized study, but the bottom line is the survival looks pretty good.— Guillermo Garcia-Manero, MD
Tweet this quote
During treatment, many patients converted from transfusion dependence to independence for red blood cells (46.4%), platelets (38.9%), or both (40.7%), for a median maximal duration of 5 months. Hematologic improvement postbaseline was observed for almost half the patients, regardless of best response achieved.
Results in Transplant Recipients
Guillermo Garcia-Manero, MD, the McCredie Professor of Medicine and Chief of the Section of MDS at The University of Texas MD Anderson Cancer Center, Houston, presented details for 51 patients who proceeded to transplantation after study treatment.2 The median time on the study drug was 124 days; the median time to transplant was 5.6 months from the first dose and 1.7 months from the last dose. For this group, azacitidine plus venetoclax led to complete responses in 41% and marrow complete responses in 45%. One patient (2%) had hematologic improvement without a response, he reported.
If you had a complete response before transplant, median overall survival was not reached at a median follow-up of 44 months; if you had a marrow complete response, median overall survival was not reached at a median follow-up of 30 months. At 2 years, estimated overall survival rates were 71% and 73%, respectively.
KEY POINTS
- Based on the benefit with azacitidine plus venetoclax in acute myeloid leukemia, this combination is being evaluated in patients with higher-risk myelodysplastic syndromes.
- Long-term results of a phase Ib trial in 107 patients demonstrated that more than 80% of patients had complete remission plus marrow complete remission.
- The duration of complete response was 16.6 months, and median overall survival was 26 months.
In an interview with The ASCO Post, Dr. Garcia-Manero commented: “The only way to cure MDS is with transplant, and you have to get patients into a deep enough response to mitigate the chance of relapse. This combination gives a higher-than-expected response rate [vs single-agent azacitidine]…. This is not a randomized study, but the bottom line is the survival looks pretty good.”
DISCLOSURE: Dr. Garcia has served as a consultant to Genentech, Servier, Gilead Sciences, Bristol Myers Squibb, Astellas, and AbbVie. Dr. Garcia-Manero reported no conflicts of interest.
REFERENCES
1. Garcia JS, Platzbecker U, Odenike O, et al: Efficacy and safety of venetoclax in combination with azacitidine for the treatment of patients with treatment-naive, higher-risk myelodysplastic syndromes. 2023 ASH Annual Meeting & Exposition. Abstract 319. Presented December 9, 2023.
2. Garcia-Manero G, Odenike O, Fleming S, et al: Combination of venetoclax and azacitidine in patients with treatment-naive, high-risk myelodysplastic syndromes with responses leading to stem cell transplantation. 2023 ASH Annual Meeting & Exposition. Abstract 1868. Presented December 9, 2023.