When President Richard M. Nixon signed the National Cancer Act into law on December 23, 1971, he said: “I hope in the years ahead, we will look back on this action today as the most significant action taken during my administration.” The increased financial investment and focus on cancer research spurred by the legislation led to a seismic shift in fundamental biologic science and understanding of the complexity of cancer and how it develops. It also fueled breakthroughs in more effective treatments of the disease, which have resulted in cures for most childhood malignancies; knowledge about how to harness the immune system against cancer; the development of life-prolonging adjuvant chemotherapy for many solid tumors; and the discovery of technologies for early detection, screening, and prevention.

Illustration by Stephanie Dalton Cowan © 2021.
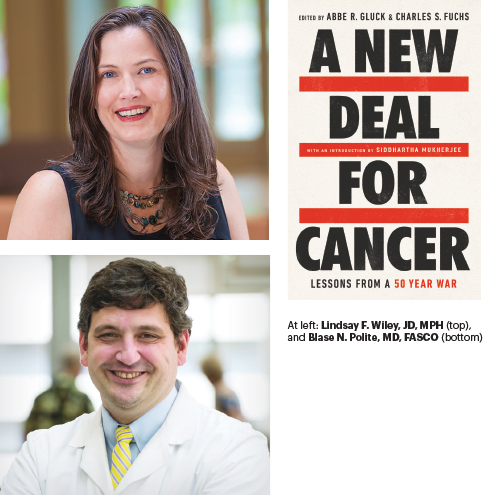
In A New Deal for Cancer: Lessons From a 50 Year War, edited by Abbe R. Gluck and Charles S. Fuchs (PublicAffairs, 2021), leaders in a variety of fields, including medicine, health law and public policy, racial justice, and medical ethics, describe the successes in the “war against cancer” over the past 50 years and the obstacles to overcome to advance a “New Deal for Cancer” over the next 50 years. (See a complete review of the book in the December 10, 2021, issue of The ASCO Post here.)
In this chapter excerpted from the book on “Cancer and Health Justice,” by Blase N. Polite, MD, FASCO, MPP, and Lindsay F. Wiley, JD, MPH, the authors argue that the U.S. health-care system is fundamentally broken and that it is a moral obligation of government to address cancer disparities, including worse survival outcomes in Black patients with cancer compared with their White counterparts. They describe an approach to eliminating racial disparities in health care, addressing how racism is systemic in the American health-care system and “functions as a social determinant of cancer disparities,” as well as how the country can build new systems that address health inequities while saving health-care costs.
This article has been excerpted from A New Deal for Cancer: Lessons From a 50 Year War, edited by Abbe R. Gluck and Charles S. Fuchs. Copyright © 2021. Available from PublicAffairs, an imprint of Perseus Books, LLC, a subsidiary of Hachette Book Group, Inc.
Cancer and Health Justice
by Blase N. Polite and Lindsay F. Wiley
Why are Black patients diagnosed with cancer at a higher rate, why are they more likely to die from cancer than their White counterparts, and how can we reverse these trends?1 However one defines health disparities, health equity, and health justice, fundamentally it comes down to questions like these. Researchers have devoted growing resources and attention to Black-white disparities in cancer outcomes for at least the last 20 to 30 years. Hundreds, if not thousands, of articles have been written on the subject. Yet we are left with an uncomfortable set of facts that for colorectal and other cancers, Black-white disparities in outcomes are actually getting worse and not better.2 The same can be said for other subordinated identities, including for people from other racial, ethnic, and cultural backgrounds; women; people living in low-income households and communities; people with disabilities; and lesbian, gay, bisexual, and transgender people. Black-white racial disparities in cancer outcomes are not necessarily the most important or the starkest among a multitude of health injustices in the United States. But disparities caused by other forms of subordination have not been subjected to the same intense, multidecade attention from researchers. For other groups and outcomes, the need for more research may forestall calls for immediate action. For Black-white cancer disparities, the research could hardly be clearer. Action is clearly long overdue for all subordinated identities, but we would argue that if the changes we recommend in this chapter are put into place, then it is likely that health equity would be achieved for other marginalized groups as well.
How can so much effort by very bright and well-meaning researchers, public health and public policy experts, and engaged community groups resulted in such a failure? The answer is that we have tried to implement incremental changes within a health-care system that is fundamentally broken and is in many ways designed to achieve this very result.
This reality is not lost on those who live under this system. A recent American Society of Clinical Oncology/Harris research poll of 4,012 adults aged 18-plus and 1,142 adults with cancer found that 71% of Black adults believe that Blacks are less likely to have access to the same quality of cancer care as whites and 27% believe race has an impact on a person’s likelihood of surviving cancer. These same beliefs were shared by 47% and 16% of white adults, respectively.
In this chapter, we will describe a health justice approach to eliminating racial disparities in health, discuss how anti-Black racism is foundational to the U.S. health system and functions as a social determinant of cancer disparities, and show concrete proof that when elected leaders prioritize health justice, we can build new systems that eliminate racial disparities while saving costs. Finally, we will propose specific changes to the existing health-care system where health justice can be imbedded as a core principle in the incentive structure as a way to achieve health equity. If our elected leaders choose not to make these changes, they should at least make it clear that the decision not to achieve health justice is a conscious one. We hope that exposing that truth will support public demands for action.
We could elaborate on health inequity and health justice for any number of cancers, such as breast, prostate, lung; hematologic malignancies; or for other health conditions, such as diabetes and cardiovascular disease, and the message from this chapter would not change: Anti-Black racism is embedded in the structural sinews of our health-care system. We instead chose to use colorectal cancer as a test case for the health justice approach. Colorectal cancer inequity has been intensely researched. More significantly, policy changes implemented in targeted geographic areas have narrowed racial disparities in key outcomes. Focusing on colorectal cancer also allows us to examine multiple failures of public health policy and the health-care system. Along the progression from community prevention to screening to diagnosis to treatment to follow-up, there are multiple points at which structural, institutional, and interpersonal racism shape outcomes.3 Focusing interventions at any one point along this pathway may achieve progress, but will ultimately fall short. In the end, achieving health justice will require fundamental changes to the entire system to dismantle the structural racism embedded in its very foundations. Specifically the system will need to (1) define, with measurable outcome metrics, what is meant by health equity; (2) hold state and local governments and private entities who are receiving trillions of health-care dollars financially accountable, at a level that they would notice, for these outcomes; and (3) adequately fund and empower community-based organizations to assist with this goal.
The Problem
Black individuals are more likely to get colorectal cancer and more likely to die from it than are their white counterparts.4 The epidemiology is not contested. More concerning is that the inequity has worsened rather than improved over the last decade. Epidemiologists from the American Cancer Society have estimated that from 2008 to 2010, more than twenty-three thousand deaths resulting from colorectal cancer could have been averted if all population groups in all states had had colorectal cancer death rates equal to the five states with the lowest death rates for the most educated whites.5 If one dismisses such an analysis as a far-fetched thought experiment, then one has to ask, why do we view it as an unattainable future? These are real body counts, not just some statistical fantasy.
The reasons for these excess deaths are multifold, but none of the reasons is without solutions. Let us start with community prevention. For colorectal cancer, there is evidence that a diet high in fat and refined grains, physical -inactivity, high glycemic load, and high body mass index all play a role in colorectal cancer incidence and, in some studies, survival from colon cancer.6 In each of these areas, Black people are more exposed to risk factors than their white counterparts.7 Environmental factors such as a lack of safe and enjoyable opportunities to be physically active; lack of access to affordable and appealing whole grains, low-fat dairy, and fresh produce; psychosocial stress; and lack of leisure time clearly contribute to these risk factors. These factors do not occur at random or as a result of individual choices unconstrained by social and physical realities. Rather, they are a clear result of historical neglect and active harm for areas with Black majority populations.8 Agricultural subsidies and other policies contribute to fresh foods’ being more expensive and more challenging to procure than refined grains and products with added sugars. Zoning, licensing, education, employment, housing, and transportation policies shape the environments in which people live, work, and make decisions about physical activity and diet.
Colorectal cancer screening saves lives. There is little to no debate about this among health-care professionals. In 2015, the American Cancer Society and the National Colorectal Cancer Roundtable set an ambitious goal of achieving 80 percent screening rates by the year 2018. Had we achieved that goal, 277,000 colorectal cancers would have been prevented and 203,000 deaths avoided. The new goal is 80 percent in every community. The longer it takes us to achieve that goal, the more deaths we will see. Black patients are less likely to be screened or to be referred for appropriate follow-up after screening than their white counterparts are, and therefore make up a disproportionate percentage of those preventable deaths. A microsimulation model estimated that differences in screening accounted for 42 percent of the disparity in colorectal cancer incidence and 19 percent of the disparity in colorectal mortality between Black and white patients.9 Differences in screening may be influenced by lack of access to health care, including lack of insurance coverage, lack of available and racially congruous providers, limited time and transportation, and discrimination against Black patients by health-care providers. Health-care providers may not spend as much time with—or offer the same recommendations to—Black patients and may treat these patients in other ways that make them reluctant to return.10
Finally, once diagnosed with cancer, lives are actually only saved by making sure the patient gets treated appropriately and in a timely fashion. Multiple studies over the last two decades have consistently shown that Black patients are less likely to receive treatment for colorectal cancer.11 At the same time, a nearly equal number of studies have shown that when Black patients are treated equally, such as occurs within a cancer clinical trial or within such settings as the Military Health System, survival outcomes are the same.12 This bears repeating: if we were to treat Blacks and whites equally, health equity would be achieved and excess deaths for Blacks would be averted. That they are not treated equally goes to the heart of why we have persistent and growing health inequities in this country. Even more gut-wrenching, Black patients may be less likely than their white counterparts to receive appropriate palliative care, including at the end of life.13
Social Determinantsof Cancer Outcomes
Achieving health justice requires inquiry and action on the full range of social determinants of poor health and premature death. In the health-care industry, the phrase “social determinants” has become something of a buzzword associated with “initiatives that buy food, offer temporary housing, or cover transportation costs for high-risk patients.”14 But these efforts to meet the immediate material needs of individual patients fall far short of meaningful action to improve the underlying social, environmental, and economic conditions that are the root causes of poor health. In the World Health Organization’s original vision, the social determinants of health “encompass [. . .] the full set of social conditions in which people live and work,” including “structural determinants” and “intermediary determinants.”15 Structural determinants of health are “social and political mechanisms that generate, configure and maintain social hierarchies.”16 Structural determinants— including racism and other forms of subordination, as well as the laws and policies in which subordination is embedded—shape the intermediary determinants of health. The intermediate determinants include material circumstances (such as housing, employment, and neighborhood factors), psychosocial circumstances, and interactions with the health system.
To put it another way, racism is a social determinant of health. It takes many forms—interpersonal, institutional, and structural. Interpersonal racism is present in interactions in which the explicit and implicit racial bias of one individual (e.g., a physician or nurse) affects other individuals (e.g., the patients they are tasked with serving).17 Institutional racism operates through the seemingly neutral practices and policies of institutions, such as hospitals and schools. Structural racism encompasses the structuring of health care, public health, education, employment, housing, and law enforcement systems to advantage people in power and subordinate racial minorities. Structural racism typically operates through laws and policies that secure racial subordination.
Anti-Black racism is deeply embedded in the core fixtures that have shaped the US health system: privatization, federalism, fiscal fragmentation, and individualism.18 One need look no further than the decision of state governments to refuse the Affordable Care Act’s expansion of Medicaid eligibility, which the Supreme Court rendered optional for states in 2012.19 As of this writing, fourteen states have made the conscious choice to reject this heavily subsidized expansion, and half of those states are clustered in the southeast. If we were to overlay a map focusing on almost any health inequity on the Medicaid expansion map, the maps would be carbon copies of each other. Six in ten Black Americans live in states that have not expanded Medicaid. The frequently cited reason is one of financial concern. Putting aside that the state liability for this expansion was limited, even that argument makes it clear that there is no desire to redistribute money from a predominantly white, higher-income majority to a Black minority population. Indeed, the decision in 1965 that, unlike Medicare, Medicaid would be jointly financed and administered by the federal government and the states has racist roots.
Social-Ecological Interventions
Health disparities are often discussed in ways that express and reinforce racist beliefs about individual blameworthiness for behaviors that are constrained by social circumstances and the supposed futility of addressing those social circumstances. Often the argument is that the fault lies with the Black individuals themselves: “If they worked harder or received more education, they would have access to private insurance and would not need the help of the state.” “If they changed their lifestyles, they would be at less risk for deadly diseases.” In other cases, rhetoric about health disparities seeks to shift blame from the health-care system to social realities that are characterized as too firmly entrenched to be amenable to intervention. “Poverty and the social determinants of health are complex and cannot be solved by elected officials.” “Health-care systems should not be penalized for poor outcomes that are attributable to social factors beyond their control.”
The notion that it is the health-care system itself, and the broader legal and political systems that are its foundation, that from birth until death ignores the needs of Black people or actively seeks to harm them, is almost never acknowledged. More broadly, we must grapple with the ways in which our health-care system reinforces, rather than confronts, privatization, federalism, fiscal fragmentation, and individualism. Finally, we must expand our focus beyond the health-care system to ensure that Black people are empowered and equipped with the resources, civil and political rights, and other legal protections they need to create health-promoting communities and secure access to healthy living and working conditions.
Empowering Communities
Central to achieving health justice is empowerment of and self-determination for Black communities and individuals. Laws and policies must be reformed to equip Black people with the legal protections and material supports they need to care for themselves, their families, and their communities. Legal protections relevant to the social determinants of health include protections from discrimination in education, employment, housing, law enforcement, and health care, and protections to ensure the safety of working and residential conditions. Financial supports include assistance with housing, food, and other basic needs. Health inequities embody the failures of our social, economic, political, and legal systems to serve all people equally. Or, to put it another way, health injustice is the result of systems of subordination that were designed to achieve it. Health justice is furthered when the tools of civil rights law—voting rights, employment and housing protections, and health-care rights—are supported by legislatures and the courts.20
Concrete Solutions
The solution is there, if we want to pursue it. We say this not as an empty statement, but because we have concrete evidence in both New York City and the state of Delaware that when achieving health equity in colorectal cancer prevention and treatment is the priority, health equity is realized. As one of us has written about elsewhere, in 2003, the New York City Department of Health and Mental Hygiene initiated the Citywide Colon Cancer Control Coalition. In addition to increasing colonoscopy screening rates for all New Yorkers, the other stated goal was to eliminate racial and ethnic screening disparities. This was achieved by crafting health messages to physicians and patients about the benefits of colonoscopy for detecting colon cancer, developing an open access colonoscopy system throughout the area allowing patients to be directly scheduled for colonoscopies without having to see a gastroenterologist for an office visit first, and providing patient navigation to make sure patients understood the colon prep and had transportation to and from the screening visit. As part of the public education campaign, the coalition recruited racially and ethnically diverse celebrity spokespeople for radio and poster campaigns to be displayed in the subway and bus shelters, created palm card distribution in check-cashing offices frequented by racial and ethnic minorities, and targeted radio campaigns to select racial and ethnic radio stations. The result, between 2003 and 2013, was an increase in colonoscopy rates from 30 to 70 percent, and the Black-white difference in screening rates was eliminated.21
The state of Delaware created a comprehensive, statewide colorectal cancer screening program with the elimination of healthcare disparities between Blacks and whites as the stated, upfront goal. The program provided coverage for colon cancer screening for the uninsured, provided patient navigation, and agreed to pay for twenty-four months of colon cancer treatment for the uninsured. Like New York, the state of Delaware also placed an emphasis on public education by partnering with over sixty community-based organizations to communicate cancer-related information. The results: between 2001 and 2009, colon cancer screening rates for both Blacks and whites reached 75 percent, colon cancer incidence rates reached parity, and the mortality rate disparity was significantly reduced. This was achieved while simultaneously saving money for the state.22
What both Delaware and New York City’s programs have in common is that they began with a primary goal of achieving health equity and then engaged a diverse set of stakeholders to help reach this goal. Certainly a key component was a centralized commitment to coordinate navigation and fund the various initiatives, but equally as important was the very early involvement of diverse stakeholders with an emphasis on community-based organizations who were empowered to come up with solutions that made the most sense for the communities they serve. While not discussed in this chapter, a not-for-profit consortium in Chicago, the Metropolitan Chicago Breast Care Task Force, was able to reduce breast cancer disparities with a similar focus. It went a step further and included the lessons learned from the lived experiences of patients who have navigated breast cancer screening to advocate for change at the state level. As a result, the task force was able to secure additional funding for the Illinois Breast and Cervical Cancer Screening Program and helped pass the Breast Cancer Excellence in Survival and Treatment Act in 2015, which put an increased focus not just on mammography access but also on the quality of mammography that women of color received. These are examples of what can be achieved when racial and ethnic minority communities are “empowered” rather than ignored or subverted. Several local governments have used their zoning and licensing authority and shared-use arrangements for public property to promote access to healthier food options and physical activity. In 2014, the Minneapolis City Council strengthened an ordinance to promote equitable access to better dietary choices in low-income neighborhoods. The ordinance requires retail food stores that are licensed as grocers to carry a minimum stock of staple foods, including fruits, vegetables, legumes, whole-grain products, and low-fat dairy products.23 Cleveland, Ohio, has launched an initiative to convert vacant properties owned by the city into appealing open spaces for physical activity and community gardening. Many cities have updated their zoning and land-use ordinances in recent years to ensure urban agriculture is permitted on public and private property.24 The Delaware Cancer Consortium has increased its focus on physical activity and nutrition and has created a “Wellness Map” that allows residents to find local farmers’ markets, where people can find fresh and local produce, as well local fitness centers, yoga studios, and parks and trails.
Finally, we have the opportunity to redesign the health-care system at the federal and state levels to make health equity a high-stakes quality metric where financial incentives flow to those who can show tangible improvements in health equity. One can start with state Medicaid programs and their contracts with the privately managed care companies that provide the majority of care for Medicaid patients in this country. Reducing if not eliminating health inequity in multiple health outcomes, from hypertension to diabetes to cancer screening and treatment, can easily be a requirement for a portion of the payments to these organizations or to the automatic assignment of patients to these plans. For example, patient assignment and/or substantial payments would be tied to the percentage of racial and ethnic minorities who have completed colon, lung, and breast cancer screening. These metrics could be expanded to include timeliness of care (time from diagnosis to definitive treatment) and ultimately to the survival of these underserved populations compared to majority patients in the state registry. Over time, as resources and patients are redistributed to those companies who do it well, this will likely incentivize the other companies to either change their strategies and methods or exit from the system. Risk-rated payments and fraud and abuse controls are critical to prevent gaming through patient selection and to not unfairly punish the organizations caring for patients with the most complex social needs, but if one organization achieves better health equity outcomes for the same group of patients compared to another, they should be rewarded for doing so. In the current system, very few real financial incentives exist to hold payers accountable for the outcomes of the patients they insure, and none that we know of specifically incentivizes health equity as a high-stakes quality outcome. Payments tied to quality are often less than 5 percent of total payments. At that level, they can be ignored as a cost of doing business. Imagine a world where they represented 50 percent of total payments—you can almost guarantee that these health-care companies would figure out how to meet the quality metrics. With our government payments, we can send a strong signal of what we hold to be important. The federal government could choose to likewise hold the states accountable for achieving health equity by tying federal match payments to this goal. While some state elected leaders may not care about the goal, they will surely care about the flow of federal funds. More fundamentally, Medicaid and other social support programs must be adequately funded at the federal level to ensure residents of states with fewer resources are not penalized for the actions of state leaders who may not be committed to serving all of their constituents equally. At the root, empowerment will require attention to the basic mechanisms of our constitutional democracy, including voting rights and other civil rights.25
The road map to achieving health equity is clear. First, the federal government and all fifty states should definitively state that achieving health equity is their goal and hold themselves accountable to a date when this will be achieved. This should be a required part of all state Medicaid plans. Second, federal and state policy makers should impose real financial incentives that will reward or penalize stakeholders in the system for their health equity outcomes, such as achieving parity in cancer screening and prevention and eventually achieving equity in cancer survival from diagnosis across a broad range of subordinated groups. Third, they should commit to adequately and equitably funding a health-care system where no individual goes without proper care because they cannot afford it. That is, they must commit to equitable health outcomes (not just health-care access) as a fundamental human right. We need to move beyond being satisfied that individuals are insured. As we are learning in the COVID-19 vaccine rollout, vaccines do not save patients, vaccinations do. Similarly, health insurance does not save people: getting high-quality, timely prevention and treatment does. This is most likely to be achieved with a national insurance funding model that obviates the need to try and set this goal at every level of our fragmented public-private health-care delivery system. Finally, federal and state leaders should adequately fund, empower, and work closely with community-based organizations to secure the living and working conditions necessary to achieve the health equity goal. These organizations know what the barriers to achieving health equity are, and in many cases they know how to solve them. They have to be given the financial resources and true stakeholder power to help put those solutions into action. To sum this up succinctly, this is how we should structure our healthcare system to actually achieve health equity:
1. Define, with measurable outcome metrics, what we mean by health equity.
2. Hold state and local governments and private entities who are receiving trillions of health-care dollars financially accountable, at a level that they would notice, for these outcomes.
3. Adequately fund and empower community-based organizations to assist with this goal. Set the incentives right and empower those who are on the front lines of this injustice, and the creative solutions will follow.
It is easy to get bogged down in the nuances of health equity research, and we can be accused of oversimplifying a complex problem. However, it is also easy to use the complexity argument as a cover for a system that has inequity as its implicit, if not explicit, goal. Coming to terms with that difficult reality is the crucial first step to actually achieving health equity. The only real question that remains is, will we?
Blase N. Polite is Professor of Medicine; Deputy Section Chief for Network and Strategy and Executive Medical Director for Cancer Accountable Care at the University of Chicago. Lindsay F. Wiley is Professor of Law and Director, Health Law and Policy Program at American University Washington College of Law.
Notes
1. American Cancer Society (ACS), Cancer Facts & Figures for African Americans 2016–2018 (Atlanta, GA: American Cancer Society, 2016).
2. Anthony S. Robbins et al., “Racial Disparities in Stage-Specific Colorectal Cancer Mortality Rates from 1985 to 2008,” Journal of Clinical Oncology 30, no. 4 (2012): 401–405, https://doi.org/10.120/JCO .2011.37.5527.
3. Ruqaiijah Yearby, “Structural Racism and Health Disparities: Reconfiguring the Social Determinants of Health Framework to Include the Root Cause,” Journal of Law, Medicine & Ethics 48, no. 3 (2020): 518–526, https://doi.org/10 .1177/1073110520958876.
4. ACS, Cancer Facts & Figures.
5. Ahmedin Jemal et al., “Inequalities in Premature Death from Colorectal Cancer by State,” Journal of Clinical Oncology 33, no. 8 (2015): 8298–35, https:// doi.org/10.1200/JCO.2014.58.7519.
6. ACS, Cancer Facts & Figures; Jeffrey A. Meyerhardt et al., “Influence of Body Mass Index on Outcomes and Treatment-Related Toxicity in Patients with Colon Carcinoma,” Cancer 98, no. 3 (2003): 484–495, https://doi.org/10 .1002/cncr.11544; Meyerhardt et al., “Physical Activity and Survival After Colorectal Cancer Diagnosis,” Journal of Clinical Oncology 24, no. 22 (2006): 3527– 3534, https://doi.org/10.1200/JCO.2006.06.0855; Meyerhardt et al., “Impact of Physical Activity on Cancer Recurrence and Survival in Patients with Stage III Colon Cancer: Findings from CALGB 89803,” Journal of Clinical Oncology 24, no. 22 (2006): 3535–3541, https://doi.org/10.1200/JCO.2006.06.0863; Meyerhardt et al., “Association of Dietary Patterns with Cancer Recurrence and Survival in Patients with Stage III Colon Cancer,” JAMA 298, no. 7 (2007): 754–764, https://doi.org/10.1001/jama.298.7.754; Meyerhardt et al., “Dietary Glycemic Load and Cancer Recurrence and Survival in Patients with Stage III Colon Cancer: Findings from CALGB 89803,” Journal of the National Cancer Institute 104, no. 22 (2012): 1702–1711, https://doi.org/10.1093/jnci/djs399.
7. ACS, Cancer Facts & Figures; Robbins, Siegel, and Jemal, “Racial Dispar-ities;” Penny M. Kris-Etherton et al., “Barriers, Opportunities, and Challenges in Addressing Disparities in Diet Related Cardiovascular Disease in the United States,” Journal of the American Heart Association 9, no. 7 (2020): e014433, https:// doi.org/10.1161/JAHA.119.014433.
8. Dayna Bowen Matthew, Just Medicine: A Cure for Racial Inequality in American Health Care (New York: New York Press, 2015).
9. Iris Lansdorp-Vogelaar et al., “Contribution of Screening and Survival Differences to Racial Disparities in Colorectal Cancer Rates,” Cancer Epidemiology, Biomarkers, and Prevention 21, no. 5 (2012): 728–736, https://doi.org/10.1158 /1055-9965.EPI-12-0023.
10. Matthew, Just Medicine.
11. Laura-Mae Baldwin et al., “Explaining Black-White Differences in Receipt of Recommended Colon Cancer Treatment,” Journal of the National Cancer Institute 97, no. 16 (2005): 1211–1220, https://doi.org/10.1093/jnci/dji241; Blase N. Polite et al., “Colorectal Cancer Model of Health Disparities: Understanding Mortality Differences in Minority Populations,” Journal of Clinical Oncology 24, no. 14 (2006): 2179–2187, https://doi.org/10.1200/JCO.2005.05.4775; Daniel R. Simpson et al., “Racial Disparity in Consultation, Treatment, and the Impact on Survival in Metastatic Colorectal Cancer,” Journal of the National Cancer Institute 105, no. 23 (2013): 1814–1820, https://doi.org/10.1093/jnci/djt318.
12. Polite et al., “Colorectal Cancer Model.”
13. Jennifer J. Griggs, “Disparities in Palliative Care in Patients with Cancer,” Journal of Clinical Oncology 38, no. 9 (2020): 974–979, https://doi.org/10.1200 /JCO.19.02108.
14. Brian C. Castrucci and John Auerbach, “Meeting Individual Social Needs Falls Short of Addressing Social Determinants of Health,” Health Affairs Blog, January 16, 2019, https://www.healthaffairs.org/do/10.1377/hblog2019 0115.234942/full/; see also Brietta R. Clark, “A Critical Race Perspective on Social Risk Targeting in the Health Care Sector,” Bill of Health Blog, October 20, 2020, https://blog.petrieflom.law.harvard.edu/2020/10/20/a-critical-race-per spective-on-social-risk-targeting-in-the-health-care-sector/#more-29370.
15. O. Solar and A. Irwin, A Conceptual Framework for Action on the Social Determinants of Health Paper 2 (Policy and Practice) (Geneva: World Health 138 Organization, 2010), 9, 27, 37, https://www.who.int/sdhconference/resources /ConceptualframeworkforactiononSDH_eng.pdf?ua=1.
16. Solar and Irwin, A Conceptual Framework for Action, 5.
17. Ruqaiijah Yearby et al., “Memo: Racism Is a Public Health Crisis. Here’s How to Respond,” Data for Progress, September 3, 2020, https://www.datafor progress.org/memos/racism-is-a-public-health-crisis.
18. Erin C. Fuse Brown et al., “Social Solidarity in Health Care, American- Style,” Journal of Law, Medicine & Ethics 48, no. 3 (2020): 411–428, https://doi .org/10.1177/1073110520958864.
19. “Status of State Action on the Medicaid Expansion Decision,” KFF.org, accessed March 22, 2021, https://www.kff.org/health-reform/state-indicator /state-activity-around-expanding-medicaid-under-the-affordable-care-act /?activeTab=map¤tTimeframe=0&selectedDistributions=status-of -medicaid-expansion-decision&sortModel=%7B%22colId%22:%22Location %22,%22sort%22:%22asc%22%7D.
20. Angela P. Harris and Aysha Pamukcu, “The Civil Rights of Health: A New Approach to Challenging Structural Inequality,” UCLA Law Review 67, no. 4 (2020): 758–832.
21. Steven H. Itzkowitz, “New York Citywide Colon Cancer Control Coalition: A Public Health Effort to Increase Colon Cancer Screening and Address Health Disparities,” Cancer 122, no. 2 (2016): 269–277, https://doi.org/10.1002 /cncr.29595.
22. Stephen S. Grubbs et al., “Eliminating Racial Disparities in Colorectal Cancer in the Real World: It Took a Village,” Journal of Clinical Oncology 31, no. 16 (2013): 1928–30, https://doi.org/10.1200/JCO.2012.47.8412.
23. “Case Studies, Minneapolis, MN,” Healthy Food Policy Project, accessed March 22, 2021, https://healthyfoodpolicyproject.org/case-studies/minneapolis -mn.
24. Ben Winig and Heather Wooten, Dig, Eat, and Be Healthy: A Guide to Growing Food on Public Property (ChangeLab Solutions, 2013), https://www .changelabsolutions.org/sites/default/files/Dig_Eat_and_Be_Happy_FINAL _20130610_0.pdf.
25. Harris and Pamukcu, “Civil Rights of Health.”

