Just in are the results of the SWOG S1007 RxPONDER trial, which evaluated the benefit of chemotherapy in women with early-stage hormone receptor–positive, HER2-negative breast cancer and node-positive disease.1 The data showed that many postmenopausal women can skip adjuvant chemotherapy, based on a 46% reduction in the risk of invasive disease–free survival events at 5 years. However, premenopausal women may still derive a benefit from adjuvant chemotherapy. Kevin Kalinsky, MD, MS, Director of the Glenn Family Breast Center at Winship Cancer Institute of Emory University, Atlanta, presented these findings at the 2020 San Antonio Breast Cancer Symposium.1

Kevin Kalinsky, MD, MS
The results somewhat echo those of TAILORx, which also sought to identify subsets of patients—with node-negative disease—who would fare well with endocrine therapy alone.2 “At the time of this analysis, our data show that postmenopausal women with hormone receptor–positive, HER2-negative breast cancer with one to three positive nodes and a 21-gene recurrence score (RS) ≤ 25 [Oncotype DX] can safely avoid receiving adjuvant chemotherapy. On the other hand, premenopausal patients with one to three positive nodes and a RS ≤ 25 should consider adjuvant chemotherapy. The invasive disease–free survival rate improved by 5% with chemotherapy in this group,” said Dr. Kalinsky.
About RxPONDER
RxPONDER aimed to determine which patients with hormone receptor–positive, HER2-negative breast cancer and one to three positive axillary lymph nodes would benefit from chemotherapy and which could safely avoid it. It is the first large, randomized trial to seek to answer this important question in this specific population.
The previous TAILORx trial was conducted in patients with hormone receptor–positive, HER2-negative breast cancer but with node-negative disease. An exploratory analysis found no chemotherapy benefit for women older than age 50 with an RS ≤ 25 vs those ≤ 50 with an RS of between 16 and 25, who did benefit.
“It’s been unclear whether the results of TAILORx can be extrapolated to women with node-positive breast cancer,” Dr. Kalinsky said.
A retrospective analysis of SWOG S8814 suggested there is a potential prognostic and predictive role of RS for chemotherapy benefit in postmenopausal patients with node-positive breast cancer. Those data formed the rationale for RxPONDER.
RxPONDER screened 9,383 women in 9 countries, ultimately including 5,015 with stage II or III breast cancer involving one to three nodes and with an RS ≤ 25. The women, two-thirds of whom were postmenopausal and one-third of whom were premenopausal, were assigned to endocrine therapy or endocrine therapy plus chemotherapy. The data were stratified by RS (0–13 vs 14–25), menopausal status, and axillary dissection vs sentinel node biopsy.
The primary endpoint was invasive disease–free survival, defined as local, regional, or distant recurrence, any second invasive cancer, or death from any cause.
5.2% Benefit in Premenopausal Subset
“TAILORx was a landmark study in patients with node-negative disease. In some ways, what we are finding is somewhat similar,” Dr. Kalinsky observed.
At a median follow-up of 5.1 years, after 54% of the anticipated events had occurred, no association was shown between chemotherapy benefit and RS values between 0 and 25 for the entire population (P = .30). A prespecified analysis, however, did find a significant association between chemotherapy benefit and menopausal status (P = .004), triggering early reporting of these data at the third prespecified interim analysis.
“Although premenopausal women with an RS between 0 and 25 had an invasive disease–free survival benefit with the addition of chemotherapy, postmenopausal women did not,” Dr. Kalinsky reported. In the premenopausal subset, the absolute benefit was 5.2% at 5 years (Table 1).
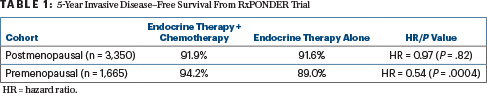
Although follow-up is still limited, especially considering these patients have hormone receptor–positive disease, at 5 years, chemotherapy also conferred a 1.3% absolute benefit in overall survival in the premenopausal cohort: 98.6% vs 97.3% (hazard ratio [HR] = 0.47; P = .032). In postmenopausal women, these survival rates were 96.2% and 96.1%, respectively (HR = 0.96; P = .79), he further reported.
Dr. Kalinsky added that the relative risk reduction for the two RS groups—0–13 and 14–25—was consistent with the overall hazard ratio of 0.54 in the premenopausal population, though the absolute benefit was numerically higher in those with RS 14–25.Consistency of benefit was also shown regardless of the number of involved nodes, though the absolute benefit varied a bit.
DISCLOSURE: Dr. Kalinsky has an immediate family member who holds stock or other ownership interests in Array BioPharma, GRAIL, and Pfizer; has served as a consultant or advisor to AstraZeneca, bioTheranostics, Cyclocel, Eisai, Genentech/Roche, Immunomedics, Ipsen, Lilly, Merck, Novartis, Pfizer, and Seattle Genetics; has participated in a speakers bureau for Lilly; has received institutional research funding from Acetylon, Amgen, Calithera Biosciences, CytomX Therapeutics, Genentech/Roche, Immunomedics, Incyte, Lilly, Novartis, Pfizer, Seattle Genetics, and Zeno Pharmaceuticals; has been reimbursed for travel, accommodations, or other expenses by AstraZeneca, Lilly, and Pfizer; and has held other relationships with Genentech and Immunomedics.
REFERENCES
1. Kalinsky K, Barlow WE, Meric-Bernstam F, et al: First results from a phase III randomized clinical trial of standard adjuvant endocrine therapy ± chemotherapy in patients with 1-3 positive nodes, hormone receptor-positive and HER2-negative breast cancer with recurrence scores ≤ 25: SWOG S1007 (RxPONDER). 2020 San Antonio Breast Cancer Symposium. Abstract GS3-00. Presented December 10, 2020.
2. Sparano JA, Gray RJ, Makower DF, et al: Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med 379:111-121, 2018.


