Data sharing between a comprehensive cancer center and a private insurer appears to be a novel way to capture practice patterns that can point to potential quality improvements. A study that combined data from Dana-Farber Cancer Institute and Blue Cross Blue Shield of Massachusetts showed that some cancer patients received intensive end-of-life care, including hospitalizations, chemotherapy, and radiation given within weeks of death.1 Moreover, the study revealed that a sizable proportion of Dana-Farber patients received care outside of Dana-Farber, including emergency department visits, hospitalizations, and radiation therapy.
Characterizing the Patterns of Care
The database included 742 patients being actively treated at Dana-Farber and with Blue Cross Blue Shield of Massachusetts as their primary insurer. The list of patients was sent to Blue Cross Blue Shield of Massachusetts, and the insurer provided available claims data for the last 6 months of life for 674 of these patients (90.8%). The median age at death was 59 years, and deaths occurred evenly in both genders.
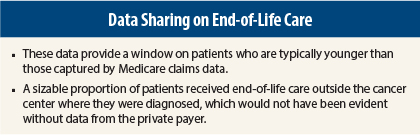
Lead author of the presentation, Sherri Oliver Stuver, ScD, of the Dana-Farber Cancer Institute in Boston, noted that these patients were younger than those typically included in Medicare claims, which have mainly been used to study end-of-life measures in cancer patients in the United States.
“Data are lacking on younger patients as well as on patients who receive part of their care outside of primary cancer centers. Our goal was to characterize the patterns of care at the end of life and thus identify strategies to improve that care,” Dr. Stuver told listeners at the 2014 ASCO Quality Care Symposium.
End-of-life National Quality Forum measures considered quality indicators were assessed in these patients. Results showed that 59.6% had any hospitalization and 47.8% had any emergency department visit within the last 30 days. Ten percent received chemotherapy in their final 14 days of life. Almost 60% received hospice care, and among those patients, 19% were treated at hospice up to 3 days before death. Intensive care unit admissions were reported in 15.4%. Death occurred in an acute care facility in 28.6% and in the intensive care unit in 10%.
“These data are fairly consistent with Medicare claims data for cancer patients. Death in the intensive care unit is certainly not an ideal occurrence,” she noted.
Other measures showed that 30.6% of patients had a red blood cell transfusion in the last 30 days of life, 8.5% had radiation therapy in the last 30 days of life, and 15.9% had surgery in the last 30 days of life.
When the investigators looked at location of care, they found that between 30% and 45% of patients received their care at facilities outside Dana-Farber or its affiliates. For example, 46% of all emergency department visits, 47% of all radiation therapy, and 30% of all hospitalizations took place outside Dana-Farber.
Putting together data like these is challenging, she continued. “These findings about care received outside of Dana-Farber highlight the benefit of merging data from cancer centers with private payers,” she emphasized.
“Going forward, it would seem that data sharing among cancer centers and payers would be a unique method for describing patterns of care,” Dr. Stuver stated. ■
Disclosure: Dr. Stuver reported no potential conflicts of interest.
Reference
1. Stuver SO, Fraile B, Donohue CC, et al: Novel data sharing between a comprehensive cancer center and a private payer to better understand care at the end of life. 2014 ASCO Quality Care Symposium. Abstract 1. Presented October 17, 2014.