The ASCO Post is pleased to present the Hematology Expert Review, an ongoing feature that quizzes readers on issues in hematology. In this installment, Drs. Abutalib and Medeiros explore extranodal marginal zone lymphoma of mucosa-associated lymphoid neoplasms (MALT lymphomas). For each quiz question that follows, select the one best answer. The correct answers and accompanying discussions appear below.
GUEST EDITORS

Syed Ali Abutalib, MD

L. Jeffrey Medeiros, MD
Dr. Abutalib is Associate Director of the Hematology and Cellular Therapy Program and Director of the Clinical Apheresis Program at the Cancer Treatment Centers of America, Zion, Illinois; Associate Professor at the Rosalind Franklin University of Medicine and Science; and Founder and Co-Editor-in-Chief of Advances in Cell & Gene Therapy. Dr. Medeiros is Professor and Chair of the Department of Hematopathology at The University of Texas MD Anderson Cancer Center, Houston.
Question 1
Which of the following statements about extranodal marginal zone lymphoma of MALT lymphomas is correct?
A. MALT lymphomas account for 15% to 20% of all B-cell lymphomas.
B. The skin is the most common site of MALT lymphoma.
C. The frequency of bone marrow involvement is higher in gastric MALT lymphomas than in nongastric cases.
D. An underlying chronic inflammatory disorder is not an uncommon finding in patients with MALT lymphoma.
Question 2
Which of the following statements about the microscopic findings of MALT lymphomas is correct?
A. These neoplasms are rarely associated with reactive follicles.
B. Neoplastic cells are generally large with abundant pale cytoplasm.
C. Neoplastic cells form characteristic lymphoepithelial lesions in gastric cases.
D. Plasmacytic differentiation is characteristically absent in MALT lymphomas.
Question 3
Which of the following statements about the immunophenotype of MALT lymphomas is correct?
A. Infrequent cases are CD5+.
B. Most cases are CD10+.
C. CD43 is always positive.
D. Noncutaneous cases express IgG heavy chains.
Question 4
Which of the following statements about the genetic profile of MALT lymphomas is correct?
A. Helicobacter pylori–associated gastric MALT lymphomas with t(11;18)(q21;q21) appear to be resistant to H pylori eradication therapy.
B. MYD88 L265P mutation is absent in MALT lymphomas.
C. TNFAIP3 abnormalities are seen in many cases of MALT lymphoma.
D. All of the above.
Question 5
Which of the following diseases can be in the differential diagnosis of MALT lymphoma?
A. Extraosseous plasmacytoma
B. Follicular lymphoma
C. Alpha heavy chain disease
D. A and B
Question 6
Which of the following infections and anatomic sites of MALT lymphoma are paired correctly?
A. Chlamydia psittaci and cutaneous MALT -lymphoma
B. Borrelia burgdorferi and alpha heavy chain disease
C. Campylobacter jejuni and ocular adnexal MALT lymphoma
D. None of the above
Answers to Hematology Expert Review Questions
Question 1
Which of the following statements about MALT lymphomas is correct?
Correct answer: D. An underlying chronic inflammatory disorder is not an uncommon finding in patients with MALT lymphoma.
Expert Perspective
MALT lymphomas account for between 7% and 8% of all B-cell lymphomas and as many as 50% of primary gastric lymphomas. The stomach (not skin) is the most common site of MALT lymphomas, affected in 35% of all cases. Other common sites include the eyes and ocular adnexa (affected in 13% of cases), skin (9%), lungs (9%), salivary glands (8%), breasts (3%), and thyroid gland (2%).1 The frequency of bone marrow involvement and involvement of multiple extranodal sites is higher in nongastric MALT lymphomas than in gastric cases. In many MALT lymphoma cases, there is a history of a chronic inflammatory condition, which results in accumulation of extranodal lymphoid tissue (called acquired MALT lymphoma). Such chronic inflammation may be the result of infection (eg, Helicobacter pylori) and/or autoimmunity (eg, Sjogren syndrome and Hashimoto thyroiditis).1
Question 2
Which of the following statements about the microscopic findings of MALT lymphomas is correct?
Correct answer: C. Neoplastic cells form characteristic lymphoepithelial lesions in gastric cases.
Expert Perspective
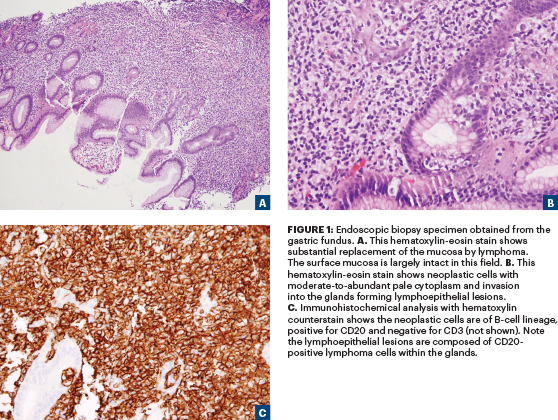
The neoplastic cells in MALT lymphomas are small- to medium-sized (Figure 1A), with inconspicuous nucleoli resembling those of centrocytes with moderate-to-abundant (not scant) pale cytoplasm (Figure 1B). The accumulation of even more pale-staining cytoplasm may lead to a monocytoid appearance, which is especially common in salivary gland MALT lymphomas. In the glandular tissues (eg, stomach), the neoplastic cells invade into the glands forming lymphoepithelial lesions, defined as aggregates of at least three marginal zone cells with distortion or destruction of the epithelium often together with eosinophilic degeneration (oxyphilic change) of epithelial cells (Figure 1C). Plasmacytic differentiation is present in approximately one-third of gastric MALT lymphomas, is frequently found in cutaneous MALT lymphomas and small intestinal MALT lymphomas (often IgA-positive), and is a constant and often striking feature in thyroid MALT lymphomas. The presence of plasmacytic differentiation may pose differential diagnosis problems with lymphoplasmacytic lymphoma.1 MALT lymphomas are commonly associated with reactive follicular hyperplasia.
Question 3
Which of the following statements about the immunophenotype of MALT lymphomas is correct?
Correct answer: A. Infrequent cases are CD5+.
Expert Perspective
The neoplastic cells of MALT lymphoma are CD20+, CD79a+, CD5–, CD10–, CD23–, CD43+/–, and CD11c+/– (weak). Infrequent cases are CD5+, and very rare cases are CD10+ but are always BCL6–. Recent reports have highlighted IRTA1 as a possible specific marker for marginal zone lymphomas, including MALT lymphomas. The neoplastic cells of MALT lymphomas typically express IgM heavy chains and less often IgA or IgG. A notable exception is cutaneous marginal zone lymphoma, of which two subsets have been described: 1) a more common class-switched subset (accounting for 75%–85% of cases) with IgG (including many IgG4+ cases) or IgA expression; and 2) usually a T-cell–predominant background and a less common (15%–25% of cases) IgM subset, which tends to be B-cell–predominant.1
Question 4
Which of the following statements about the genetic profile of MALT lymphomas is correct?
Correct answer: A. Helicobacter pylori–associated gastric MALT lymphomas with t(11;18)(q21;q21) appear to be resistant to H pylori eradication therapy.
Expert Perspective
The frequencies at which the translocations or trisomies (most commonly +3 and +18) occur vary markedly with the primary site of disease, but none of these abnormalities are specific for MALT lymphoma.1
The t(11;18)(q21;q21) translocation is mainly detected in pulmonary and gastric tumors. H pylori–associated gastric MALT lymphomas with t(11;18)(q21;q21) appear to be resistant to H pylori eradication therapy. The t(14;18)(q32;q21) translocation is mainly detected in ocular adnexa, orbit, and salivary gland lesions; and the t(3;14)(p14.1;q32) translocation is mainly detected in MALT lymphomas arising in the thyroid gland, ocular adnexa, orbit, and skin.1-3 The t(1;14)(p22;q32) translocation is associated with MALT lymphomas arising in the intestines, salivary glands, and lungs. MYDBB L265P mutation has been reported in 6% to 9% of MALT lymphomas. Abnormalities of TNFAIP3 on chromosome 6q23, which may include deletions, mutations, and promoter methylation, occur in 15% to 30% of cases, most frequently cases lacking specific translocations. TNFAIP3 abnormalities are not specific for MALT lymphomas.1-3
Question 5
Which of the following diseases can be in the differential diagnosis of MALT lymphoma?
Correct answer: D. A and B.
Expert Perspective
In some MALT lymphomas, there is a marked predominance of plasma cells, resulting in resemblance to an extramedullary plasmacytoma requiring careful examination to accurate diagnosis. Amyloid deposition is seen in some cases of MALT lymphomas. Myeloid cell nuclear differentiation antigen staining may facilitate the differential diagnosis of MALT lymphoma vs follicular lymphoma,
because this nuclear antigen is expressed in 61% to 75% of MALT lymphomas but less than 10% of follicular lymphomas. Chronic lymphocytic leukemia and mantle cell lymphoma should be excluded in CD5+ cases of MALT lymphoma.1 Alpha heavy chain disease, also known as immunoproliferative small intestinal disease, is a variant of MALT lymphoma in which defective IgA heavy chains are secreted.4
Question 6
Which of the following infections and anatomic sites of MALT lymphoma are paired correctly?
Correct answer: D. None of the above.
Expert Perspective
MALT lymphomas arising at any anatomic site share many characteristics, but there are also site-specific differences with respect to etiology, morphologic features, molecular cytogenetic abnormalities, and clinical course. A role for antigenic stimulation by Chlamydia psittaci, Borrelia burgdorferi, and Campylobacterjejuni has been proposed for some cases of ocular adnexal MALT lymphoma, cutaneous MALT lymphoma, and alpha heavy chain disease, respectively. In the early phase, alpha heavy chain disease (immunoproliferative small intestinal disease) may completely remit with antibiotic therapy. In patients with more advanced disease, multiagent chemotherapy is typically required.
DISCLOSURE: Dr. Abutalib is an advisor for AstraZeneca and has served on the advisory board of Jazz Pharmaceuticals. Dr. Medeiros reported no conflicts of interest.
REFERENCES
1. Cook JR, Isaacson PG, Chott A, et al: Extranodal marginal zone lymphoma of mucosal-associated lymphoid tissue (MALT lymphoma), in Swerdlow SH, Campo E, Harris NL, et al (eds.): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, pp 259-262. Lyon France, International Agency for Research in Cancer, 2017.
2. Streubel B, Huber D, Wohrer S, et al: Frequency of chromosomal aberrations involving MALT1 in mucosa-associated lymphoid tissue lymphoma in patients with Sjögren’s syndrome. Clin Cancer Res 10:476-480, 2004.
3. Remstein ED, Dogan A, Einerson RR, et al: The incidence and anatomic site specificity of chromosomal translocations in primary extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) in North America. Am J Surg Pathol 30:1546-1553, 2006.
4. Cook JR, Harris NL, Isaacson PG, et al: Heavy chain disease, in Swerdlow SH, Campo E, Harris NL, et al (eds.): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, p 240. Lyon, France, International Agency for Research in Cancer, 2017.

