As low-dose computed tomography (CT) screening for lung cancer has moved from clinical trials to clinical practice, management issues are growing more urgent for screening centers around the country: for instance, how to support referrals from and to other providers; how to ensure the quality of scans; how to handle findings of other diseases?

Screening is a demanding, complex management process.— James L. Mulshine, MD
Tweet this quote
“Screening is a demanding, complex management process,” said James L. Mulshine, MD, of Rush University Medical Center, opening the 14th Quantitative Imaging Workshop in Washington, DC. This year’s workshop explored successful strategies to streamline the management process and overcome obstacles, encouraging integration of low-dose CT screening by the larger medical community; creating an infrastructure designed to ensure the quality of images obtained from various screening instruments; and effectively managing tobacco-related findings on low-dose CT scans, including early signs of chronic obstructive pulmonary disease (COPD) and cardiovascular disease.
The annual Quantitative Imaging workshops, convened by the Prevent Cancer Foundation, provide a forum to exchange ideas on quantitative CT imaging for early disease management, as well as on policy and advocacy for lung cancer, COPD, and cardiovascular screening. “There are many different edges—different perspectives and challenges,” said Carolyn Aldigé, President and Founder of the Foundation. “We’re talking about a world that doesn’t exist yet, utilities that are just nascent. It is incredibly challenging.”

We’re talking about a world that doesn’t exist yet, utilities that are just nascent. It is incredibly challenging.— Carolyn Aldigé
Tweet this quote
Medical Community Acceptance
In a recent survey by the Lung Cancer Alliance, almost half of respondents in its Screening Centers of Excellence reported that “lack of support from referring providers” was a continued barrier to low-dose CT screening.
Amy Copeland, Director of Medical Outreach at the Lung Cancer Alliance, presented the survey results, which included some of the first data on the implementation of low-dose CT screening since it was approved for individuals at high risk of lung cancer. (The U.S. Preventive Services Task Force [USPSTF] approved it in 2013, and the Centers for Medicare & Medicaid Services [CMS], in 2015, for older adults who have a 30 pack-year smoking history and who currently smoke or have quit within the past 15 years.)
Lung Cancer Alliance Screening Centers of Excellence—now numbering 526 centers in 42 states—are committed to responsible, high-quality screening practices. Survey respondents from 137 health systems reported 30,819 baseline screenings and 11,702 follow-up scans in 2016.

Amy Copeland
The survey data confirmed anecdotal evidence that, in general, primary care providers have been slow to embrace low-dose CT screening. Low-dose CT for early lung cancer while approved by the USPSTF and virtually all other lung cancer–related professional groups is not recommended by the American Academy of Family Physicians, citing concerns about false-positive findings, the risks of radiation exposure from annual follow-up scans, and the risks of follow-up surgery.
It’s true that many providers don’t think the benefits of low-dose CT justify those risks, said David Yankelevitz, MD, PhD, of the Icahn School of Medicine at Mount Sinai, a long-time low-dose CT researcher who is affiliated with the International Early Lung Cancer Action Program (I-ELCAP). That idea stems from a misunderstanding of the extent of the benefit of screening based on the findings of the National Lung Screening Trial (NLST), he said in an interview.

The 20% reduced mortality in the [NLST] results does not translate directly into the actual proportion of lives that can be saved by regular low-dose CT screening of high-risk groups. That proportion is much higher.— David Yankelevitz, MD, PhD
Tweet this quote
In the NLST, patients screened with low-dose CT had a relative reduction in mortality from lung cancer of 20% compared to the control group, which received traditional chest x-rays. That benefit is often described as “marginal.” But the 20% does not refer solely to cancers diagnosed during the trial, Dr. Yankelevitz pointed out. It includes all lung cancer deaths that occurred during long-term follow-up, including deaths from cancers diagnosed after the screening portion of the trial ended.
“The 20% reduced mortality in the trial results does not translate directly into the actual proportion of lives that can be saved by regular low-dose CT screening of high-risk groups,” he said. “That proportion is much higher.”
Another factor in provider reluctance to refer patients is the time required. “Primary care providers already have a lot on their plate,” said Ms. Copeland. “Adding more tasks related to screening is difficult, especially the CMS requirement for counseling and shared decision-making.” The Lung Cancer Alliance is now developing strategies to alleviate the extra burden, such as by providing screening centers with tools to reach out to primary care providers.
Radiologists also have been slow to adopt low-dose CT. Again, time is one reason—the scans are detailed and time-consuming to interpret. Also, reporting requirements are complex and reimbursement is low, Dr. Yankelevitz said. One hopeful trend, he added, is the growing use of software packages to analyze the scans. Better integration of them into the workflow could make a difference.
Other barriers reported by the Lung Cancer Alliance centers included insurance and billing issues, lack of patient awareness, and, less often, lack of patient interest. Administrative issues—internal workflow and staff/time limitations—were also cited frequently.
COPD and Cardiovascular Disease
Another management issue stems from the frequent findings of markers for COPD and cardiovascular disease during low-dose CT screening. In the Lung Cancer Alliance survey, more than half of respondents reported frequent “incidental” findings of COPD/emphysema and coronary artery calcification. The Lung Cancer Alliance survey found that most centers refer these patients back to their primary care providers, whereas others refer to a specialist. Some simply inform patients of the findings.
“What stood out from the data was that there’s no standardized way these ‘incidental’ findings are being managed,” said Ms. -Copeland. “It’s not the screening that saves a life; it’s getting that person into timely and appropriate care once something has been found, whether it is lung cancer or another treatable condition.”
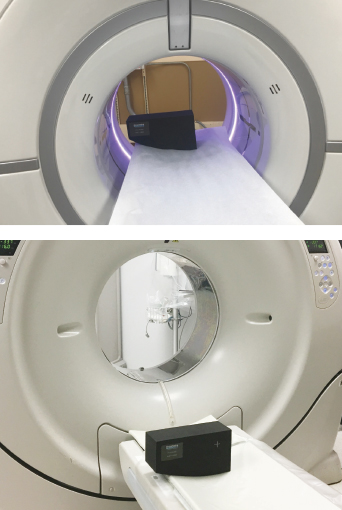
These photos show the phantom used for the QIBA Small Nodule Conformance evaluation of CT imaging quality. The goal of the evaluation is to confirm that the CT scan is functioning correctly, with the appropriate settings to allow the acquisition of a thoracic CT scan and with sufficient resolution to ensure the quantitative assessment for early lung cancer is based upon high-quality imaging data.
The Lung Cancer Alliance is planning to study workflows and offer guidance on best follow-up practices. “This is where our value lies as an organization—having the potential to bridge the gap between screening and care, creating and improving the continuum,” she said.
Scans showing signs of COPD and coronary artery calcification raise larger management questions as well. Integrating COPD and coronary artery calcification into lung cancer screening makes sense: The same populations are at risk, and all three diseases are major public health problems. Preventing them, through detection of early imaging markers and systematic management, principally with lifestyle interventions, has the potential to save many millions of dollars in projected health-care costs as the population ages.
However, oncologists, cardiologists, and pulmonologists do not usually work together on research or care delivery, noted Dr. Mulshine. How to integrate prevention, screening, and care for all three diseases is an important, unaddressed question for the medical community, he said.
Quality Assurance
A third major theme at this year’s workshop was how to ensure the quality of images. Diagnosis of lung cancer by low-dose CT depends on accurate measurement of changes in the size of lung nodules over time; the quality of the images is crucial.
“The main quality issue stems from variability among scanners,” said Ricardo Avila, Chief Executive Officer of Accumetra, LLC, speaking at the workshop. “The fundamental reason for variability is that scanners have many parameter settings, and their trade-offs are not known.”

The fundamental reason for variability [among scanners is that they] have many parameter settings, and their trade-offs are not known.— Ricardo Avila
Tweet this quote
Accumetra is working on a pilot project with the Quantitative Imaging Biomarkers Alliance (QIBA), organized by the Radiological Society of North America, to develop a system that would provide the tools to ensure that high-quality quantitative CT measurements are being performed at clinical sites.
The system features a phantom, or test object, that can be used to calibrate the settings of a CT scanner. Using the cloud, radiologists upload an image of the phantom taken with their own equipment and receive feedback within minutes on how it compares to requirements in the QIBA CT Small Lung Nodule Profile. (The profile which has just received consensus approval by the QIBA committee, provides specifications and requirements for CT measurement of volume change in small solid lung nodules.) Based on the report, radiologists can adjust equipment settings if needed and submit new scans to verify conformance with the QIBA Profile.
In a pilot study in 2016, Accumetra found much variability among screening sites and scanners used to measure identical phantoms—in that case, rolls of adhesive tape. Now a more sophisticated phantom, made with materials and manufacturing methods used by the aerospace industry, is ready for testing. With support from the Prevent Cancer Foundation, Accumetra is distributing 80 of the new phantoms to U.S. and international screening sites for further testing.
QUANTITATIVE IMAGING WORKSHOP XIV
- Held October 2–3 in McLean, Virginia
- Organized by the Prevent Cancer Foundation
- Theme: Lung Cancer, COPD, and Cardiovascular Disease
- Supported by Genentech
“If successful, the system could lead to the first small-nodule change measurement conformance service,” Mr. Avila said. That in turn could lead to a national or international infrastructure to support quality standards for screening devices—a primary concern for the low-dose CT screening community.
The ultimate goal, said Dr. Mulshine, is for “better, less expensive, faster implementation of cloud-enabled low-dose CT screening of the three leading causes of tobacco-related premature death—lung cancer, COPD, and cardiovascular disease.” ■
DISCLOSURE: Dr. Mulshine, Ms. Copeland, and Ms. Aldigé reported no conflicts of interest. Mr. Avila is owner and Chief Executive Officer of Accumetra, LLC. Dr. Yankelevitz is a named inventor on a number of patents and patent applications relating to the evaluation of diseases of the chest, including measurement of nodules. Some of these, which are owned by Cornell Research Foundation (CRF) are nonexclusively licensed to General Electric. As an inventor of these patents, Dr. Yankelevitz is entitled to a share of any compensation that CRF may receive from its commercialization of these patents. He is also a consultant and shareholder for Accumetra, LLC, and on the advisory board for Grail.

