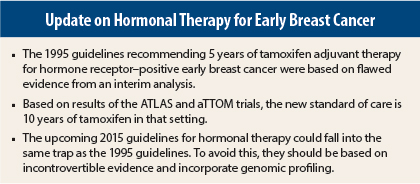
Guidelines can be incorrect if they are not based on incontrovertible evidence. Such was the case with the National Cancer Institute (NCI) 1995 guidelines recommending 5 years of tamoxifen adjuvant therapy for stage I to III hormone receptor–positive breast cancer. With more definitive evidence, ASCO issued 2014 guidelines recommending 10 years of tamoxifen as the new standard.
In 2015, new guidelines on aromatase inhibitors and gonadotropin-releasing hormone agonists are expected, and these guidelines could fall into a similar trap as the NCI 1995 guidelines for tamoxifen, according to Norman Wolmark, MD, Chairman of the National Surgical Adjuvant Breast and Bowel Project (NSABP) and Professor and Chairman of Human Oncology at the Drexel University School of Medicine, Philadelphia.
He stated that the new guidelines should incorporate genomic profiling; otherwise they will miss the mark.
“Hormonal management of adjuvant therapy of breast cancer justifies a reprise. Are we destined to learn from the mistakes of the past, or are we going to repeat them?” was the challenge Dr. Wolmark issued in his Keynote Address at the 2014 Chemotherapy Foundation Symposium.1
Mistakes of the Past
The 1995 NCI guidelines for adjuvant tamoxifen, distributed to every oncologist at every U.S. hospital, were based on results of a 7-year interim analysis of the NSABP 14 protocol, which evaluated the use of adjuvant tamoxifen for 5 years vs 10 years for breast cancer. At 7 years, 5 years looked like it was superior, but this analysis failed to account for the rebound effect that continues after stopping tamoxifen. The study was stopped because it crossed futility limits.
“What a mistake!” he exclaimed. “This set us back a decade.”
More recently, data from the ATLAS and aTTOM trials showed a 4% incremental benefit for 10 years of tamoxifen compared with 5 years (hazard ratio = 0.80).2,3
“The ATLAS and aTTOM trials were unencumbered by interim analyses—they plotted on and went forward. This refuted the NSABP 5-year gold standard,” he stated. The new ASCO guidelines recommend 10 years of total tamoxifen therapy.
Dr. Wolmark suggested that the new guidelines may be “authoritarian,” and there may be cohorts for whom 10 years of hormonal therapy is not desirable. Perhaps these cohorts could be identified by genomic signatures such as Oncotype DX that determine which patients are at risk for early or late tumor recurrence.
Resurgence of Luteinizing Hormone-Releasing Hormone Agonists
“New data that have emerged in the past 2 years exacerbate the dilemma of how to address the enigma of the ovary. Some of these therapeutic strategies are competing and mutually exclusive,” Dr. Wolmark told listeners. “We may be deluding ourselves if we have conflicting data and think that we will find a Rosetta stone,” he said.
Several trials suggest that gonadotropin-releasing hormone agonist analogs and luteinizing hormone-releasing hormone analogs can reduce the risk of tumor recurrence in premenopausal women with hormone receptor–positive breast cancer.
“These agents are making a comeback in premenopausal women. They have been tried before. It’s like being on a roller coaster,” Dr. Wolmark said. “2014 is the year of resurgence of luteinizing hormone-releasing hormone agonists.”
Data are conflicting about whether tamoxifen plus ovarian function suppression (ie, with gonadotropin-releasing hormone agonist or luteinizing hormone-releasing hormone agonists) or aromatase inhibitor plus ovarian function suppression has a greater effect on reducing tumor recurrence in premenopausal women.
Updated results of a joint analysis of the TEXT and SOFT salvage trials should provide further evidence of this question. These results will be presented at the 2014 San Antonio Breast Cancer Symposium. A previous joint analysis favored ovarian function suppression plus exemestane over tamoxifen plus ovarian function suppression, with a 5% absolute difference in disease-free survival at 5.7 years of follow-up.4
“Are we going to think this is a home run? I’m not holding my breath,” he said.
Hypothetically, the 2015 guidelines could state that premenopausal women should be offered an aromatase inhibitor with gonadotropin-releasing hormone agonist for 5 years. He questions this, as well as the duration of therapy beyond 5 years whether they remain premenopausal or become postmenopausal.
He suggested there may be premenopausal cohorts who can benefit from 5 vs 10 years of this type of therapy. Additional trials will show the optimal duration of aromatase inhibitors (NSABP-42) and disease-free survival with ovarian function suppression (MA17R).
“Strap yourselves into that roller coaster,” he said.
Take-Home Message
“The take-home message is that if the data are definitive and incontrovertible, go ahead and formulate guidelines. On the other hand, we are in the era of genomic profiling. Do the guidelines apply to every patient, in this age of molecular genomics? If the guidelines don’t take into account genomic profiling, you may miss the mark. You can run the risk of paying an enormous price and setting back the field by at least a decade,” Dr. Wolmark stated. ■
Disclosure: Dr. Wolmark reported no potential conflicts of interest.
References
1. Wolmark N: 2014 Chemotherapy Foundation Symposium. Presented November 5, 2014.
2. Davies C, et al: Lancet 381:805-816, 2013.
3. Gray RG, et al: 2013 ASCO Annual Meeting. Abstract 5.
4. Pagani O, et al: 2014 ASCO Annual Meeting. Abstract LBA1.