I found my cancer quite accidentally. In March 2018, as I was taking a shower, my hand casually brushed against my right mastoid bone, and I noticed the area sounded hollow. Around the same time, I realized I had developed a sense of fullness in that ear as well. I had been feeling tired, but that was easily explained by running after two young daughters, ages 3 and 2, and having recently moved from Australia to outside London. Still, I decided to have my ear examined and was assured by an ear, nose, and throat specialist that my problem was most likely caused by a sinus infection.
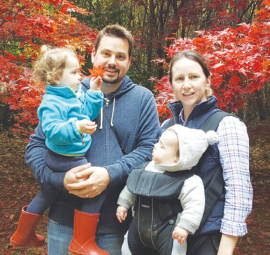
Tina Marin with her husband, Justin, and daughters, Remy (left) and Ellery.
When my husband, children, and I made a trip home to The Woodlands, Texas, for a family visit, I saw my primary care physician for additional tests, and the results were normal. It wasn’t until I developed a ferocious headache on the right side of my head while on a hiking trip in the Canary Islands that I knew something was seriously wrong.
Back in London, I made an appointment with a neurologist who suggested I undergo magnetic resonance imaging of my skull, which showed a large mass that had eroded my mastoid bone and was pressing on my brain. After the neurosurgeon performed a biopsy of the tumor, it was determined I had non–germinal center/activated B-cell–type diffuse large B-cell non-Hodgkin lymphoma. My research skills in epidemiology kicked in, and I learned I was dealing with an aggressive subtype that does not respond as well to standard-of-care chemotherapy as other types of non-Hodgkin lymphomas.
Searching for a Cure
I believe in research and, at age 35, with the prospect of no longer being around for my husband and our two young children, I wanted to see whether there was an appropriate clinical trial that might increase my chances for a cure. We quickly moved our family back to Texas, and I met with Jason Westin, MD, Assistant Professor in the Department of Lymphoma and Myeloma and Head of the Diffuse Large B-Cell Lymphoma Research Team at The University of Texas MD Anderson Cancer Center. Dr. Westin was enrolling newly diagnosed patients with my type of diffuse large B-cell lymphoma in a phase II trial investigating a combination of targeted therapy that included rituximab, lenalidomide, and ibrutinib, followed by standard chemotherapy with rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.1
Although I am mentally prepared to live in the moment and enjoy each day, I hope this clinical trial has given me the chance to be part of many more future moments and days with my family.— Tina Marin
Tweet this quote
It is not an exaggeration to say that the day after my initial treatment with rituximab, it felt like there was a war going on in my head. Three days later, my hearing returned in my right ear. After just two cycles of the combination therapy, I felt fine. I didn’t have any adverse events, was able to resume my normal life, and could take my daughters to their preschool.
An interim positron-emission tomography (PET) scan showed that I had a robust partial response to the therapy. Subsequent PET scans after completion of cycle two of six cycles of the chemotherapy combined with rituximab, lenalidomide, and ibrutinib found no evidence of disease.
Staying Connected in Life
I don’t mean to make what I went through over the past year sound easy. It wasn’t. I had to be hospitalized every 21 days while undergoing treatment and at one point for a neutropenic fever I developed, which meant being isolated from my family while in the hospital. Even at home, I quarantined myself in my room to reduce the risk of additional infections. The hardest part for me during this time was not adjusting to the fact that I had a life-threatening cancer that could shorten my life but was watching and listening to the outside world go on without me.
I still get emotional when I think about those days in the hospital or ensconced in my room, unable to see or touch my children. I’m sure it was a confusing time for them. I know it was a devastating time for me. My older daughter made cards for me every day. While in the hospital, I was able to FaceTime twice a day with my daughters, and that helped keep me connected in their young lives.
My family took on the task of caring for the girls, my husband, and me on a daily basis. I am forever grateful for the love, support, and positive energy they created around me.
Finding Acceptance
We were very happy living abroad and are still adjusting to life back home and finding our new “normal” here. The course of my life and the lives of my family have been irrevocably altered by cancer, and we are still dealing with the aftermath of my illness and finding our way forward. I don’t look at my diagnosis as a positive or negative event. It is just a fact of my life that I live with every day.
As part of the clinical trial protocol, I am monitored every 3 months for signs of relapse, so I haven’t had a chance yet to put cancer behind me and move ahead with plans for my future. In some ways, that is a good thing, because before my diagnosis, I wasn’t living in the present. Although I am mentally prepared to live in the moment and enjoy each day, I hope this clinical trial has given me the chance to be part of many more future moments and days with my family.
This is my new reality, and I’ve accepted it. ■
Ms. Marin, 36, lives in The Woodlands, Texas.
Editor’s Note: Columns in The Patient’s Corner are based solely on information The ASCO Post received from patients and should be considered anecdotal.
REFERENCE
1. Westin J, Nastoupil LJ, Fayad L, et al: Smart start: Final results of rituximab, lenalidomide, and ibrutinib lead in prior to combination with chemotherapy for patients with newly diagnosed diffuse large B-cell lymphoma. 2019 ASCO Annual Meeting. Abstract 7508. Presented June 4, 2019.

