Studies in triple-negative breast cancer presented at the 2014 ASCO Annual Meeting sought to determine predictors of response to platinum agents. One identified a subset of responders to neoadjuvant chemotherapy, but prediction proved more elusive in metastatic disease.
Neoadjuvant Carboplatin
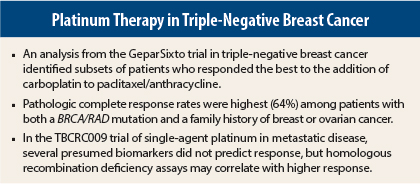
The addition of carboplatin to neoadjuvant chemotherapy mainly benefits triple-negative breast cancer patients with either a family history of breast or ovarian cancer or a germline BRCA or RAD51C/D mutation, according to an analysis of the GeparSixto study presented by Gunter von Minckwitz, MD, PhD.1
“Compared to patients with no risk factors, pathologic complete response rates tended to be higher in patients with a family history or a genetic alteration, but were highest when both factors were present,” said Dr. von Minckwitz, Chairman of the German Breast Group and Professor of Gynecology at the University of Frankfurt.
“Without these risk factors, the gain in pathologic complete response was only marginal, 11%,” he said.
The GeparSixto analysis of germline status and family history “might help identify patients with higher benefit from using carboplatin as part of neoadjuvant chemotherapy, to justify the associated increase in toxicity,” he said.
As background, Dr. von Minckwitz noted that triple-negative breast cancer patients, especially those with BRCA mutations, are sensitive to DNA-damaging agents; that deleterious germline or somatic mutations, not only of BRCA1/2 but also RAD51C/D, predict high platinum sensitivity in ovarian cancer; and that the addition of carboplatin to anthracycline/taxane-based chemotherapy can increase pathologic complete response rates in triple-negative patients.
The randomized phase II GeparSixto study further explored these findings by evaluating the effect of carboplatin added to weekly paclitaxel and nonpegylated liposomal doxorubicin in 595 patients with triple-negative or HER2-positive breast cancer. The main results, recently published,2 showed pathologic complete response rates increased by 33% when carboplatin was added (P = .17; P = .2 was the level of statistical significance in GeparSixto), but the effect was completely derived from the subgroup of triple-negative patients, whose odds of pathologic complete response increased by 94% and who achieved a complete response rate of 53.2% (P = .005).
Germline Status and Family History
Dr. von Minckwitz presented an analysis of response to carboplatin in 294 patients, using a conservative definition of pathologic complete response (ypT0, ypN0). As a secondary endpoint, the group also evaluated response according to germline BRCA/RAD mutations and family history of breast or ovarian cancer. About 14% of patients had BRCA1/2 mutations, 1% had RAD50/51C alterations, and 34% had a relevant family history.
The pathologic complete response rate was 40% for patients without mutations or family history, 49% for those with a family history, 55% for those with genetic alterations, and 64% for patients with both family history and genetic alteration, he reported.
“By the more commonly used definition for pathologic complete response, which includes cases of ductal carcinoma in situ, the group with two factors present had a pathologic complete response rate that increased to 81.8%,” he added.
The absolute gain in pathologic complete response with the addition of carboplatin was highest in those with family history (+27%) and germline alterations (+23%). Without risk factors, the gain was minimal (11%). The analysis is ongoing, and additional BRCA mutations will be found, he said.
Biomarkers in Metastatic Setting
Steven J. Isakoff, MD, PhD, of Massachusetts General Hospital and Harvard Medical School, Boston, reported that established biomarkers were unable to predict response to platinum therapy in patients with metastatic triple-negative breast cancer in the TBCRC009 study.3
TBCRC009 was a single-arm multicenter phase II study evaluating platinum monotherapy (carboplatin or cisplatin) in the first- or second-line treatment of 86 metastatic triple-negative breast cancer patients. The study found that platinum monotherapy was active in sporadic and BRCA1/2-associated disease.
Response rates varied notably by germline BRCA1/2 status, with responses observed in 54.5% of BRCA carriers compared to 19.7% of wild-type patients (P = .022). However, BRCA1/2 status did not predict for longer progression-free or overall survival.
“A meaningful subset of patients achieved durable responses and remain progression-free for over 4 years, but durable responses were not associated with a BRCA1/2 mutation,” he said.
Neither response nor durable response was predicted by p63/p73 expression, p53/PIK3CA mutation, or molecular subtype. “Caution, therefore, is necessary when evaluating biomarkers developed in the pretreatment setting for use in metastatic disease,” he commented. ■
Disclosure: Drs. von Minckwitz and Isakoff reported no potential conflicts of interest. For full disclosures of all study authors, visit meetinglibrary.asco.org.
References
1. von Minckwitz G, Hahnen E, Fasching PA, et al: ASCO Annual Meeting. Abstract 1005. Presented June 3, 2014.
2. von Minckwitz G, Schneeweiss A, Loibl S, et al: Lancet Oncol 15:747-756, 2014.
3. Isakoff SJ, He L, Mayer EL, et al: ASCO Annual Meeting. Abstract 1020. Presented June 3, 2014.