The American Association for Cancer Research (AACR) and The Mark Foundation for Cancer Research recently announced five grants to support innovative research focused on understanding the influence of a patient’s biology on the genesis, development, treatment, and survivorship of cancer. Each Science of the Patient grant will provide $750,000 over 3 years to support projects that explore novel concepts with the potential to have transformative impacts on future clinical practice.
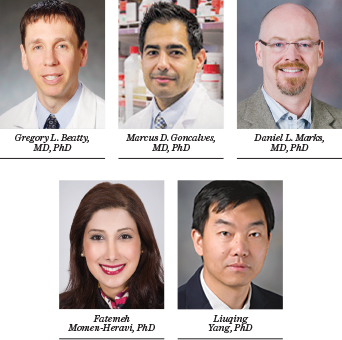
The recipients are:
Gregory L. Beatty, MD, PhD, of the University of Pennsylvania. “Impact of Liver Biology on Cancer Immunity” will study how the liver affects cancer immunotherapy efficacy. The goals of this project are to define determinants of the liver response to human cancer and to interrogate mechanisms by which the liver coordinates immune dysfunction. In doing so, Dr. Beatty aims to identify novel therapeutic targets and new treatments for patients with cancer.
Marcus D. Goncalves, MD, PhD, of Weill Cornell Medicine. “Targeting Insulin to Improve Endometrial Cancer” will use mouse models and data from human clinical trials to test whether a very low carbohydrate diet reduces tumor insulin signaling, increases markers of cell death, and enhances the efficacy of PI3K inhibitors in endometrial cancer.
Daniel L. Marks, MD, PhD, of Oregon Health & Science University. “Autonomic Dysfunction in Cancer Cachexia” will investigate pathways originating in the brain that lead to cachexia, the debilitating condition involving weight loss, muscle wasting, adipose tissue reprogramming, and anorexia found in approximately 80% of patients with pancreatic ductal adenocarcinoma. Better understanding these pathways may potentially provide novel therapeutic options for cachexia, including drugs that are already used in clinical practice or advanced clinical trials. These same pathways are implicated in enhanced risk of tumor growth and metastasis, which suggests that blocking these responses may also provide synergistic benefit with tumor-directed therapeutics.
Fatemeh Momen-Heravi, PhD, of Herbert Irving Comprehensive Cancer Center at Columbia University. “Biological Mechanism and Risk Factor of Head and Neck Cancer in Blacks” aims to characterize the molecular features of head and neck squamous cell carcinoma and identify transcriptomic changes associated with the disease in patients with African ancestry. Pathway analysis and integration of omics data will be used to uncover tumor vulnerabilities in Black patients for therapeutic intervention, with the ultimate goal of developing personalized therapies and reducing health disparities.
Liuqing Yang, PhD, of The University of Texas MD Anderson Cancer Center. “Liver PAH Defect Provokes Immune Resistance” will focus on the molecular mechanism of immunotherapy-associated liver impairment and its effects on a patient’s metabolic microenvironment and acquired resistance to immunotherapy. Findings may influence current clinical management and pave the way for treatments targeting liver function to overcome acquired resistance.

