The relationship between margin width and risk of recurrence after breast-conserving surgery for ductal carcinoma in situ depends on the use of radiation, according to a surgical oncologist who sought to determine the optimal margin width in these patients.1 “Positive margins are associated with an increased risk of local recurrence, but there is no consensus regarding the optimal negative margin width,” said Kimberly Van Zee, MD, FACS, of Memorial Sloan Kettering Cancer Center, New York.
The other important question concerns the use of radiation therapy, which appears to cut locoregional recurrences by half but does not affect mortality and does carry some risk. No subset of patients with ductal carcinoma in situ has been identified for whom radiation therapy does not reduce the rate of recurrence, but the reduction is proportional. “There is interest in identifying those at low risk, who have a small absolute risk reduction from radiation,” she revealed.
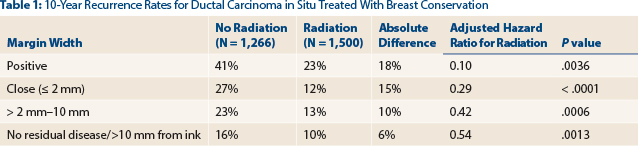
The study she reported at the 2016 Miami Breast Cancer Conference may help. In the study, Dr. Van Zee and colleagues analyzed a large prospective database of patients with ductal carcinoma in situ with long follow-up, examining the risk of recurrence with various margin widths, analyzed separately for those who did and did not receive radiation.2 Their conclusion was that wider negative margins are especially important for reducing the risk of recurrence in patients who do not receive radiation, and radiation therapy is especially important when patients have close or positive margins.

Kimberly Van Zee, MD, FACS
In short, said Dr. Van Zee, “The benefit of radiation is smaller in patients with wide margins, and wider negative margins may not be necessary in women undergoing radiation.”
Lessons Not Learned From EBCTCG Analysis
As background, Dr. Van Zee described the Early Breast Cancer Trialists’ Collaborative Group’s (EBCTCG’s) analysis of four randomized trials of adjuvant radiotherapy after breast-conserving surgery for ductal carcinoma in situ. The 10-year recurrence rates were approximately double in patients who did not receive radiation, both for negative- and positive-margin groups; the positive-margin cohort, in the absence of radiation, had a recurrence rate of 43.8%.3
Similarly, in a large Swedish trial, radiation reduced the risk of recurrence at 20 years by roughly half for patients with either negative or positive margins.4 Patients with negative margins had substantially better outcomes than those with positive margins, in both those who did and did not receive radiation.
“While these studies clearly showed that negative margins are better than positive, the optimal margin width was not addressed, and the definition of negative margin was defined differently in different studies,” admitted Dr. Van Zee.
Surgical Margin Width and Radiation Therapy in Breast Cancer
Among women not receiving radiation after breast-conserving surgery for ductal carcinoma in situ, wider margins are associated with a lower risk of recurrence. Among those not receiving radiation, progressive decreases in risk of recurrence were linked to wider margins, culminating in a risk reduction of 69% among patients who demonstrated no residual disease or margins > 10 mm from ink (P < .0001). The data suggest that patients not receiving radiation need wider margins. The use of radiation is associated with a lower risk of recurrence for all margin widths.Therefore, there remains no consensus for optimal margin width. Based on a conference of experts this past November, a draft consensus statement about ductal carcinoma in situ management was developed and is currently being reviewed by specialty societies. Due to a lack of data about margin width in the absence of radiation, it will not contain a recommendation for that scenario, acknowledged Dr. Van Zee.
“Our aim was to evaluate the relationship between margin width in ductal carcinoma in situ, adjusting for other factors that also affect recurrence risk and stratifying by the use of radiation,” she said.
Their prospective database included 2,996 patients with ductal carcinoma in situ who had breast-conserving surgery between 1978 and 2010 and were followed for a median of 75 months. They examined age (as a continuous variable), family history, presentation, number of excisions, nuclear grade, use of radiation, endocrine therapy, and year of surgery.
Margin widths were categorized as shown here (7% of cases were unknown):
- Positive: 0 mm from ink (3%)
- Close: ≤ 2 mm from ink (15%)
- Intermediate: > 2 mm to 10 mm from ink (30%)
- No residual disease in reexcision specimen or > 10 mm from ink (45%)
Ten-year recurrence rates for the whole population were 31% for those with positive margins, 17% for those with close margins, 18% for those in the intermediate group, and 13% for those with no residual disease or > 10 mm from ink. “We saw some separation of the Kaplan-Meier curves, but the differences did not reach statistical significance,” she noted.
A multivariable model adjusted for seven factors that also impact risk and determined the independent effect of margin width. As compared to positive margins, wider negative margins were associated with a progressively lower hazard ratio (HR) for recurrence as follows: close (HR = 0.78), intermediate (HR = 0.70), and no residual disease/> 10 mm (HR = 0.44; P = .0003).
“The hazard ratio associated with wider margins progressively fell, with a 56% reduction in risk associated with the widest margin, vs a positive margin,” concluded Dr. Van Zee.
Among the No-Radiation Group, Reduced Risk of 69%
Among those not receiving radiation, margin width was even more strongly associated with recurrence. Using multivariable analysis to adjust for other factors, progressive decreases in risk were observed with wider margins, culminating in a risk reduction of 69% among patients who demonstrated no residual disease or margins > 10 mm from ink (P < .0001). “In contrast, among patients receiving radiation, there was no significant association, even after adjusting for other variables,” Dr. Van Zee said.
“Looking at the same data another way—for radiation vs no radiation according to margin width—among those with positive or close margins, the difference between patients receiving radiation and not receiving it is large, whereas among those with wider margins, the difference with radiation is much smaller. For every margin group, the hazard ratio associated with radiation was highly significant,” she noted (Table 1, page 16).
Despite the limitations of this study, continued Dr. Van Zee, “there does seem to be a differential effect of margin width on recurrence, depending on the use of radiation…. The absolute reduction in the risk of recurrence associated with radiation is larger when you have positive or close margins and smaller when you have wider margins.” ■
Disclosure: Dr. Van Zee reported no potential conflicts of interest.
References
1. Van Zee K: What is the current definition of clear margin in DCIS? 2016 Miami Breast Cancer Conference. General Session. Presented March 11, 2016. (download brochure to view presentations)

