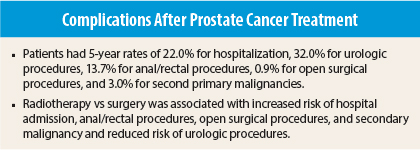
Studies of complications of surgery or radiotherapy for prostate cancer generally focus on incontinence and erectile dysfunction. In a population-based cohort study reported in The Lancet Oncology, Robert Nam, MD, MSc, FRCS(C), Professor of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, and colleagues assessed the frequency of other complications related to such treatment and found high rates of hospitalization, urologic procedures, anal/rectal procedures, open surgeries, and, in those receiving radiotherapy, secondary malignancies.1 Radiotherapy was associated with higher rates of hospitalization, anal/rectal procedures, open surgical procedures, and secondary malignancy and a lower rate of urologic procedures vs surgery.
Study Details
The study included administrative hospital data, physician billing codes, and cancer registry data from 32,465 men who received either radical prostatectomy (n = 15,870), surgery, or radiotherapy alone (n =16,595) for prostate cancer between 2002 and 2009 in Ontario. Five-year rates of treatment-related hospital admissions, urologic procedure, anal/rectal procedures, open surgical procedures, and secondary malignancies were identified. Rates were compared with those in a control group of men without history of prostate cancer drawn from a health insurance database who were matched (1:1) for age and year of treatment/inception.
Patients undergoing surgery were significantly younger (median, 62 vs 70 years, P < .0001; 42% vs 13% < 60, 50% vs 37% 60–70, and 7% vs 49% > 70 years, P < .0001 for trend) and had significantly lower comorbidity scores using Johns Hopkins ACG Case-Mix System sum of aggregated disease groups scoring (P < .0001).
Complication Rates
Among all patients, the 5-year cumulative incidence of admission to hospital for a treatment-related complication was 22.2%, with 2.4% of patients having a stay longer than 1 day. Five-year rates were 32.0% for urologic procedures, 13.7% for anal/rectal procedures, 0.9% for open surgical procedures, and 3.0% for second primary malignancies.
The most common urologic procedure was cystoscopy (62% of procedures in the radiotherapy group and 58% in the surgery group). The most common causes of hospitalization were radiation proctitis in the radiotherapy group (41% of admissions) and urinary obstruction in the surgery group (70%). The most common anal/rectal procedure was lower gastrointestinal endoscopy (67% of procedures in the radiotherapy group and 82% in the surgery group). The most common open surgical procedures were genitourinary/gastrointestinal fistula repair (36% of procedures) and open bladder neck repair (27%) in the radiotherapy group and cystotomy (76%) in the surgery group.
The most common sites of secondary malignancy were gastrointestinal (27% of all sites) and lung (25%) in the radiotherapy group and gastrointestinal (25%), genitourinary (20%), and hematologic (20%) in the surgery group.
Comparison With General Population
After adjustment for age, comorbidity, and year of inception, patients had significantly elevated risk vs the general population for hospital admission (hazard ratio [HR] = 17.9, P < .0001), urologic procedures (HR = 6.8, P < .0001), anal/rectal procedures (HR = 2.2, P < .0001), and open surgical procedures (HR = 6.0, P < .0001).
Among patients receiving radiotherapy, there was a significantly greater rate of second malignancy vs expected cancers in the general population among all patients (standardized incidence ratio [SIR] = 2.0, 95% confidence interval [CI] = 1.7–2.3) and among those aged between 40 and 65 years (SIR = 3.5, 95% CI = 2.3–4.7) and a no significant increase was found among those aged 65 to 90 years (SIR = 0.8, 95% CI = 0.7–1.0).
Among patients undergoing surgery, there was no significant increase among all patients (SIR = 0.8, 95% CI = 0.6–1.0), a nonsignificant increase among those aged between 40 and 65 years (SIR = 1.3, 95% CI = 0.9–1.8), and a significant reduction among those aged 65 to 90 years (SIR = 0.4, 95% CI = 0.3-0.6).
Factors Associated With Increased Risk
On multivariate analysis, older age and higher comorbidity score were associated with increased risk of minimally invasive urologic procedures (HR = 1.01, P < .0001; HR = 1.08, P < .0001), hospital admission (HR = 1.007, P < .0001; HR = 1.08, P < .0001), anal/rectal procedures (HR = 1.02, P = .011; HR = 1.10, P < .0001), and secondary malignancy (HR = 1.04, P < .0001; HR = 1.04, P < .0001).
The single most important predictor for complications was the type of index treatment patients underwent. Patients receiving radiotherapy vs surgery had significantly greater risk for admission to hospital during years 2 to 5 (HRs = 1.62-10.8, P < .0001 for all) with a reduced risk during year 1 (HR = 0.86, P < .0001), significantly increased risk of rectal/anal procedures (HR = 2.72, P < .0001) and secondary malignancy (HR = 2.08, P < .0001), and increased risk of open surgery in years 2 to 5 (HRs = 1.53-3.68, P = .002 for year 2, P < .0001 for years 3–5). Risk of urologic procedures was reduced in patients receiving radiotherapy (HR = 0.66, P < .0001).
The investigators concluded, “Complications after prostate cancer treatment are frequent and dependent on age, comorbidity, and the type of treatment. Patients and physicians should be aware of these risks when choosing treatment for prostate cancer, and should balance them with the clinical effectiveness of each therapy.” ■
Disclosure: The study was supported by the Ajmera Family Chair in Urologic Oncology and by the Institute for Clinical Evaluative Sciences, which is funded by the Ontario Ministry of Health and Long-Term Care. The study authors reported no potential conflicts of interest.
Reference
1. Nam RK, Cheung P, Herschorn S, et al: Incidence of complications other than urinary incontinence or erectile dysfunction after radical prostatectomy or radiotherapy for prostate cancer: A population-based cohort study. Lancet Oncol 15:223–231, 2014.