Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) accounts for approximately 5% of Hodgkin lymphoma cases. It is distinguished from classic Hodgkin lymphoma by a variety of clinical and pathologic features, including expression of B-cell associated antigens such as CD20. Given that the overall prognosis in limited-stage NLPHL is extremely good, the goals of therapy should be to maintain high cure rates and avoid future secondary complications, similar to the treatment goals in limited-stage classic Hodgkin lymphoma. Classic Hodgkin lymphoma is typically treated with a combined-modality approach consisting of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) or ABVD-like chemotherapy and radiation therapy. Optimal treatment for limited-stage NLPHL has not yet been defined.
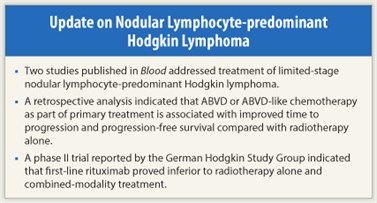
Two studies of treatment of limited-stage NLPHL were recently published in the journal Blood. A retrospective analysis by Savage and colleagues1 indicated that ABVD or ABVD-like chemotherapy as part of primary treatment is associated with improved time to progression and progression-free survival compared with radiotherapy alone. A phase II trial reported by Eichenauer and colleagues2 in the German Hodgkin Study Group indicated that although first-line treatment with the anti-CD20 antibody rituximab (Rituxan) appears to be inferior to radiotherapy alone and combined-modality treatment, investigation of combination approaches including anti-CD20 antibody treatment in NLPHL is warranted.
Retrospective Analysis of ‘RT Era’ vs ‘ABVD Era’
Savage and colleagues analyzed outcomes in patients in the British Columbia Cancer Agency Lymphoid Cancer Database with limited-stage NLPHL (stage IA/IB or IIA, nonbulky disease < 10 cm) who were treated prior to 1993 with radiotherapy alone (RT era, n = 32) and another group treated after 1993, generally with two cycles of ABVD-like therapy followed by radiotherapy (ABVD era, n = 56).1 Of 56 ABVD era patients, 14 did not receive radiotherapy and 6 received only radiotherapy. Four ABVD era patients received MOPP (mechlorethamine, vincristine, procarbazine, prednisone) plus ABV. One RT era patient received MOPP. Most patients were male (75% in each group), most were aged 40 years or younger (62.5% of RT era patients and 61% of ABVD era patients), most had stage I disease (66% and 59%, respectively), and mass size was 5 cm or smaller (72% and 66%, respectively) in most patients with measurements.
In the total patient group, there were no significant differences between patients with stage I disease and those with stage II disease with regard to 10-year time to progression (88% vs 88%) or progression-free survival (74% vs 88%). Univariate analysis showed no impact on progression-free survival for male sex, age greater than 49 years, or mass greater than 5 cm.
ABVD Bests Radiotherapy Alone
 Patients treated in the ABVD era had markedly better long-term outcomes than those in the RT era, including a markedly reduced incidence of relapse and transformation to aggressive lymphoma. Median follow-up for living patients was 6.4 years (range, 1.2–40.5 years). For patients treated in the ABVD era, 10-year time to progression was increased from 76% to 98% (P = .0074), progression-free survival from 65% to 91% (P = .0024), and overall survival from 84% to 93% (P = .07) compared with those treated in the RT era. The only lymphoma relapse observed in ABVD era patients was in a patient who received RT alone. In contrast, with a median time to progression of 5.3 years, there were 12 relapses in RT era patients, including 5 cases of transformation to aggressive lymphoma.
Patients treated in the ABVD era had markedly better long-term outcomes than those in the RT era, including a markedly reduced incidence of relapse and transformation to aggressive lymphoma. Median follow-up for living patients was 6.4 years (range, 1.2–40.5 years). For patients treated in the ABVD era, 10-year time to progression was increased from 76% to 98% (P = .0074), progression-free survival from 65% to 91% (P = .0024), and overall survival from 84% to 93% (P = .07) compared with those treated in the RT era. The only lymphoma relapse observed in ABVD era patients was in a patient who received RT alone. In contrast, with a median time to progression of 5.3 years, there were 12 relapses in RT era patients, including 5 cases of transformation to aggressive lymphoma.
An “as treated” analysis comparing outcomes in patients who received chemotherapy in either era as part of primary treatment (n = 51, median follow-up of living patients, 5.7 years) vs those receiving radiotherapy alone in either era (n = 35, median follow-up of living patients, 18.6 years) showed a significantly greater 10-year progression-free survival rate among patients receiving chemotherapy (100% vs 77.5%, P = .0029). No relapses occurred in the chemotherapy patients, compared with 10 among those receiving RT alone. Most relapses in the radiotherapy-alone patients occurred within 5 years of diagnosis.
Rituximab in Newly Diagnosed Stage IA NLPHL
In a single-arm phase II trial conducted by Eichenauer and colleagues,2 28 evaluable patients with newly diagnosed stage IA NLPHL received four weekly infusions of rituximab at 375 mg/m2. Patients had a median age of 40 years, 71% were male, and 72% had supradiaphragmatic disease. After diagnostic lymph node biopsy, 39% of patients were in complete remission and 61% had residual disease.
At a median follow-up of 43 months, the overall response rate was 100%, with complete remission in 86% and partial remission in 14%. Progression-free survival estimates at 12, 24, 36, and 48 months were 96%, 85%, 81%, and 77%, respectively. Relapse occurred in seven patients (25%), and two developed secondary solid tumors. All relapses occurred in patients with residual disease after diagnostic lymph node resection. No grade 3 or 4 adverse events were observed.
As noted by the investigators, although the response rate with rituximab in first-line treatment was excellent—as are response rates with rituximab in relapsed or more advanced disease—the 25% relapse rate after a median 43-month follow-up does not compare well with outcomes reported for radiotherapy alone or combined-modality treatment.
Earlier Investigations
In a German Hodgkin Study Group retrospective analysis of 131 patients with early-stage disease receiving radiotherapy alone or combined-modality therapy, the freedom from treatment failure rate at 43 months was 95%.3 A single center analysis of 113 patients with stage I or II disease receiving radiotherapy alone showed a 5-year progression-free survival of 95% with a median follow-up of 136 months for living patients. However, secondary malignancy was the main cause of death in this group.4
The authors noted that “anti-CD20 antibodies have a favorable toxicity profile and may be offered to young patients who are at particular risk for long-term side effects, such as secondary malignancies. In addition, the combination of anti-CD20 antibodies and chemotherapy may also improve efficacy and decrease toxicity of NLPHL treatment in early unfavorable, advanced, or relapsed disease.”2 ■
References
1. Savage KJ, Skinnider B, Al-Mansour M, et al: Treating limited-stage nodular lymphocyte-predominant Hodgkin lymphoma similarly to classical Hodgkin lymphoma with ABVD may improve outcome. Blood 118:4585-4590, 2011.
2. Eichenauer DA, Fuchs M, Pluetschow A, et al: Phase 2 study of rituximab in newly diagnosed stage IA nodular lymphocyte-predominant Hodgkin lymphoma: A report from the German Hodgkin Study Group. Blood 118:4363-4365, 2011.
3. Nogova L, Reineke T, Eich HT, et al: Extended field radiotherapy, combined modality treatment or involved field radiotherapy for patients with stage IA lymphocyte–predominant Hodgkin’s lymphoma: A retrospective analysis from the German Hodgkin Study Group (GHSG). Ann Oncol 16:1683-1687, 2005.
4. Chen RC, Chin MS, Ng AK, et al: Early-stage lymphocyte-predominant Hodgkin’s lymphoma: Patient outcomes from a large, single-institution series with long follow-up. J Clin Oncol 28:136-141, 2010.

