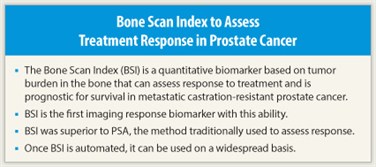
Researchers at Memorial Sloan-Kettering Cancer Center have developed the Bone Scan Index (BSI), which is the first quantitative imaging response biomarker that can assess response to treatment and prognosticates for survival in men with metastatic castration-resistant prostate cancer.
Based on Bone Scintigraphy
 “We have shown for the first time that it is possible to develop a quantitative imaging response biomarker for assessing treatment effects in bone. The BSI, which is based on bone scintigraphy, can express as a single number the amount of disease progression or regression as a result of treatment for patients with metastatic castration-resistant prostate cancer,” said Michael J. Morris, MD, of Memorial Sloan-Kettering Cancer Center, New York. Dr. Morris is senior author of this study, which was recently published in the Journal of Clinical Oncology.1
“We have shown for the first time that it is possible to develop a quantitative imaging response biomarker for assessing treatment effects in bone. The BSI, which is based on bone scintigraphy, can express as a single number the amount of disease progression or regression as a result of treatment for patients with metastatic castration-resistant prostate cancer,” said Michael J. Morris, MD, of Memorial Sloan-Kettering Cancer Center, New York. Dr. Morris is senior author of this study, which was recently published in the Journal of Clinical Oncology.1
Prior to development of the Bone Scan Index, there was no reproducible or quantifiable way to describe responses using bone scans. As Dr. Morris explained, bone scintigraphy is an imperfect tool that images the bone, not the cancer itself, and for which there are few standard descriptors of post-treatment changes.
“The bone scan shows the derivative effect on the bone surrounding the metastasis,” he said. “And we do not have a standard quantitative expression that tells us whether a patient is responding to treatment. The BSI is such an expression. It is a single quantitative output that describes all the lesions in a patient’s body, rising or falling depending on how a patient is responding to treatment. These post-treatment fluctuations prognosticate for survival.”
 The Bone Scan Index is a method of expressing the tumor burden in bone as a percentage of the total skeletal mass based on “reference man” skeletal masses. (Created in 1974 by the International Commission on Radiological Protection, reference man provides a standard set of biologic characteristics modeled on a hypothetical young Caucasian male.) The study describes an association between BSI and survival. Bone scans of 88 men with metastatic castration-resistant prostate cancer who were enrolled in four clinical trials were analyzed to calculate BSI at baseline and 3 and 6 months on treatment. The percent change in BSI from baseline to 3 and 6 months was prognostic for survival. A doubling in BSI was associated with almost a twofold increase in risk of death.
The Bone Scan Index is a method of expressing the tumor burden in bone as a percentage of the total skeletal mass based on “reference man” skeletal masses. (Created in 1974 by the International Commission on Radiological Protection, reference man provides a standard set of biologic characteristics modeled on a hypothetical young Caucasian male.) The study describes an association between BSI and survival. Bone scans of 88 men with metastatic castration-resistant prostate cancer who were enrolled in four clinical trials were analyzed to calculate BSI at baseline and 3 and 6 months on treatment. The percent change in BSI from baseline to 3 and 6 months was prognostic for survival. A doubling in BSI was associated with almost a twofold increase in risk of death.
Compared with PSA
When Bone Scan Index was compared with prostate-specific antigen (PSA)—the traditional method of determining response to treatment—change in PSA was not prognostic for survival.
“We compared PSA head-to-head with BSI, and found that BSI was a more accurate indicator of treatment benefit,” Dr. Morris stated. “Even older imaging modalities like bone scintigraphy can be analyzed correctly and developed as quantitative imaging biomarkers that capture important survival information, and appear to be superior to traditional methods like PSA.”
Dr. Morris and colleagues are now working on automating the Bone Scan Index so that it is computer-generated instead of being computed manually. “When that automation is ready for prime time, every clinician out there will be able to use BSI as a response biomarker,” he stated. ■
Disclosure: Dr. Morris reported no potential conflicts of interest.
Expert Point of View: New Biomarker Predicts Survival in Advanced Prostate Cancer
Reference
1. Dennis ER, Jia X, Stephenson RD, et al: Bone scan index: A quantitative treatment response biomarker for castration-resistant metastatic prostate cancer. J Clin Oncol. January 9, 2012 (early release online).

