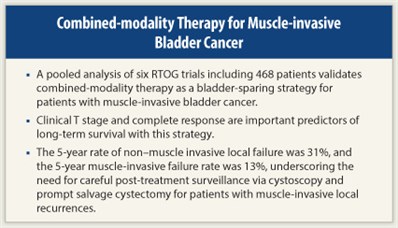
 Combined-modality therapy provides a bladder-sparing alternative to radical cystectomy with comparable outcomes in patients with muscle-invasive bladder cancer, according to a pooled analysis of six Radiation Therapy Oncology Group (RTOG) trials.1 The study included 468 patients and showed that clinical T stage and complete response are important predictors of long-term survival in patients with muscle-invasive bladder cancer who undergo combined-modality therapy.
Combined-modality therapy provides a bladder-sparing alternative to radical cystectomy with comparable outcomes in patients with muscle-invasive bladder cancer, according to a pooled analysis of six Radiation Therapy Oncology Group (RTOG) trials.1 The study included 468 patients and showed that clinical T stage and complete response are important predictors of long-term survival in patients with muscle-invasive bladder cancer who undergo combined-modality therapy.
“Combined-modality therapy can spare the bladder, but the optimal [chemoradiation] regimen for [this approach] remains to be defined. The small sample sizes of these [six] studies do not allow comparisons between these trials to determine optimal combined-modality therapy,” said Raymond H. Mak, MD, of the Harvard Radiation Oncology Program, Boston, at the 2012 Genitourinary Cancers Symposium.
The six trials were RTOG 8802, 8903, 9506, 9706, 9906, and 0233; five were phase II trials and one was a phase III study. These small trials all utilized combined-modality therapy with a variety of neoadjuvant and/or adjuvant regimens. Two trials included two cycles of neoadjuvant chemotherapy, one trial had no neoadjuvant or adjuvant chemotherapy, and three incorporated adjuvant chemotherapy.
Study Details
 The analysis was based on a total of 468 patients with a median age of 66 years; 64% were younger than age 70, 19% were aged 70 to 75, and 17% were older than age 75. Among all patients, 82% were male. Approximately 94% had transitional cell carcinoma; 61% had clinical stage T2 tumors, and 35% had clinical stage T3. Median follow-up was 4.3 years for all patients and 7.8 years among 205 survivors.
The analysis was based on a total of 468 patients with a median age of 66 years; 64% were younger than age 70, 19% were aged 70 to 75, and 17% were older than age 75. Among all patients, 82% were male. Approximately 94% had transitional cell carcinoma; 61% had clinical stage T2 tumors, and 35% had clinical stage T3. Median follow-up was 4.3 years for all patients and 7.8 years among 205 survivors.
Seventy-two percent of patients had a complete response to combined-modality therapy. The 5- and 10-year estimated overall survival rates were 57% and 36%, respectively; 5- and 10-year estimated disease-specific survival rates were 71% and 65%.
The majority of local failures in the bladder were non–muscle invasive, with an estimated 5- and 10-year incidence of 31% and 36%. The 5- and 10-year estimates for muscle-invasive failure rates were 13% and 14%, and 5- and 10-year estimates of distant metastases were 31% and 35%.
“This recurrence pattern underscores the need for careful post-treatment surveillance via cystoscopy [with prompt salvage cystectomy for invasive tumor recurrences] and further study for novel systemic therapies,” Dr. Mak told listeners. Patients with a complete response to combined-modality therapy had improved 5-year survival vs nonresponders: 79% vs 56%.
Multivariate analysis adjusted for age and histology found that higher clinical T stage (cT3/4 vs cT2) was associated with decreased overall and disease-specific survival. Elderly (age ≥ 75) patients did not have significantly different disease-specific survival compared with younger (age 70-75 and age < 70) patients (64% vs 61% vs 67% at 10 years, respectively), Dr. Mak explained. Thus, the pooled data from these multi-institutional prospective trials indicate that bladder-preserving chemoradiation is a good treatment option for elderly patients, and satisfies an unmet need for treatment options in this group of patients, many of whom (30%-40% are not receiving curative treatment).2 ■
Disclosure: Dr. Mak reported no potential conflicts of interest.
Expert Point of View: Study Shows Concurrent Chemoradiation Therapy to be a Viable Strategy for Muscle-invasive Bladder Cancer
References
1. Mak RH, Hunt D, Shipley WU, et al: Long-term outcomes in patients with muscle-invasive bladder cancer after bladder preserving combined-modality therapy: A pooled analysis of RTOG 8802, 8903, 9706, 9906, and 0233. Genitourinary Cancers Symposium. Abstract 264. Presented February 3, 2012.
2. Gray PJ, Fedewa SA, Shipley WU, et al: Receipt of aggressive therapies for muscle-invasive bladder cancer: Results from the National Cancer Data Base. Genitourinary Cancers Symposium. Abstract 272. Presented February 3, 2012.

 According to Seth P. Lerner, MD, Professor in the Scott Department of Urology at Baylor College of Medicine, Houston, and Co-chair of the session at the Genitourinary Cancers Symposium where the study by Mak and colleagues was presented, the data clearly demonstrate proof of principle that the...
According to Seth P. Lerner, MD, Professor in the Scott Department of Urology at Baylor College of Medicine, Houston, and Co-chair of the session at the Genitourinary Cancers Symposium where the study by Mak and colleagues was presented, the data clearly demonstrate proof of principle that the...