 Results from the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial, which found no benefit for completion axillary nodal dissection in patients with breast cancer involving one to two positive sentinel nodes,1 have led to changes in breast cancer management, though points of discussion remain. In an interview with The ASCO Post, Barbara L. Smith, MD, PhD, a surgical oncologist and Director of the Breast Program at Massachusetts General Hospital, Boston, offered her perspective on some of the key issues and remaining questions regarding sentinel node biopsy and axillary surgery in 2012.
Results from the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial, which found no benefit for completion axillary nodal dissection in patients with breast cancer involving one to two positive sentinel nodes,1 have led to changes in breast cancer management, though points of discussion remain. In an interview with The ASCO Post, Barbara L. Smith, MD, PhD, a surgical oncologist and Director of the Breast Program at Massachusetts General Hospital, Boston, offered her perspective on some of the key issues and remaining questions regarding sentinel node biopsy and axillary surgery in 2012.
Accuracy of Sentinel Node Mapping
How confident can clinicians be today that sentinel node mapping is effective?
Success rates with sentinel node–mapping range from 95% to 99%, with false-negative rates generally less than 10%. In three studies that provided data from sentinel node biopsy and axillary lymph node dissection, the percentage of node-positive patients was essentially the same with either approach.2-4 Outcomes from such studies have confirmed that sentinel node mapping accurately identifies node-positive patients and is therefore an effective staging tool.
What is the rate of axillary failure after a negative sentinel node biopsy?
Long-term follow-up of some of these same studies showed that axillary recurrence rates are extremely low in patients with a negative sentinel node biopsy, and are no higher after sentinel node biopsy alone than after axillary lymph node dissection. Axillary recurrence rates were 0.4% with dissection and 0.7% with sentinel node biopsy in the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32 trial,2 and 0% and 0.8%, respectively, in the Veronesi study.4 Overall survival was also similar, at 90% to 93%, respectively.
Why would the axillary recurrence rates be so low, if the false-negative rate with sentinel node biopsy is about 10%?
We know that not all positive axillary nodes will progress and become clinically significant. Also, sentinel node–positive patients often receive tangent radiation to cover the axilla, which sterilizes tumor deposits, and patients almost always receive systemic therapy, which we know contributes to local control.
Role of Local Therapy
What happens if these additional components of treatment are eliminated?
 This is an important question, because it applies to patients with negative sentinel nodes who have mastectomy without radiation, or, increasingly, have accelerated partial breast irradiation rather than whole-breast irradiation.
This is an important question, because it applies to patients with negative sentinel nodes who have mastectomy without radiation, or, increasingly, have accelerated partial breast irradiation rather than whole-breast irradiation.
We looked at this at our institution in 487 clinically node-negative patients who underwent sentinel node biopsy, with a median of two nodes removed, then underwent mastectomy.5 There were 365 patients with negative sentinel nodes (n = 325) or isolated tumor cells only (n = 40), and none received radiation. Systemic therapy was given to all patients with invasive cancers and to 35% who underwent mastectomy for ductal carcinoma in situ. At 70 months follow-up, recurrences were observed in only two patients with negative sentinel nodes (0.6%) and in none of the patients with isolated tumor cells, even though these patients did not receive radiation. Both relapses were in patients with extensive high-grade ductal carcinoma in situ who did not receive systemic therapy.
These data and data from mastectomy patients suggest that negative sentinel nodes really do not need additional local therapy. But, importantly, most patients in these studies received systemic therapy, which is likely a major contributor to local control in sentinel node biopsy patients.
So, to sum up, what can be concluded about negative sentinel nodes?
Large randomized trials solidly confirm that a negative sentinel node biopsy provides staging and prognostic information equivalent to a negative axillary lymph node dissection. Survival after a negative sentinel node biopsy is equivalent to survival after a negative axillary dissection. For clinically node-negative patients, sentinel node biopsy is the standard of care for staging.
Occult Metastasis
How concerned should clinicians be about nodes containing isolated tumor cells, which can’t be classified as “positive” or “negative”?
A key part of sentinel node biopsy is enhanced pathologic assessment, usually with serial sections and immunohistochemistry. These techniques can identify very small tumor deposits that traditional H&E staining can miss. But how frequently is the sentinel node found to be immunohistochemistry-positive after it’s been shown to be H&E-negative? In other words, what is the frequency of occult sentinel node metastasis?
In ACOSOG Z0010, the rate was 10%,6 and in NSABP B-32, it was about 16%.7 ACOSOG Z0010 assessed the impact of these occult metastases and found that survival at 5 years was significantly lower in patients with H&E-positive sentinel nodes (93%) than in those with H&E-negative nodes (96%; P = .0002). However, when stratifying the H&E-negative nodes by immunohistochemistry status, no difference in overall survival was shown (95% vs 96%; P = .53).6 The investigators concluded that tumor deposits identified only on immunohistochemistry had no impact on prognosis in patients as they are currently treated.
And in B-32,7 a significant reduction in overall, disease-free, and distant disease-free survival was shown, but the absolute magnitude of the differences was extremely small. The 5-year overall survival difference was just 1.2%. The authors concluded that occult metastases were an independent prognostic factor, but that there was no clinical benefit to routine immunohistochemistry in H&E-negative sentinel nodes. Nodal staging should be based on the size of the metastatic deposit, not the means of detection.
Who Requires Axillary Dissection?
For patients with a positive sentinel node, when is axillary dissection necessary?
It used to be standard for a patient with a positive sentinel node to have complete axillary lymph node dissection, but ACOSOG Z0011 showed otherwise. Patients in the Z0011 trial had clinical N0, T1-2 tumors, H&E-detected sentinel node metastases, lumpectomy with whole-breast irradiation, and adjuvant systemic therapy. For patients meeting the eligibility criteria, the local recurrence risk was remarkably low after sentinel node biopsy only. At a median follow-up of 6.3 years, the local (in-breast) recurrence rate was 3.6% after axillary lymph node dissection and 1.8% after sentinel node biopsy. Regional node recurrence rates were 0.5% and 0.9%, respectively, and total locoregional recurrence rates were 4.1% and 2.8%, respectively (P = .11). Overall and disease-free survival rates were also not significantly different.
At the 2011 San Antonio Breast Cancer Symposium, we heard confirmation of these findings in an update of the International Breast Cancer Study Group Trial 23-01 (see sidebar).8 The study compared axillary lymph node dissection and sentinel node biopsy alone and found no difference in 5-year disease-free survival (88% per arm). The axillary relapse rate was only about 1% after sentinel node biopsy.
ACOSOG Z0011 concluded that for clinically node-negative patients who have one or two positive sentinel nodes and undergo radiotherapy and systemic therapy, the routine use of axillary node dissection is no longer justified, but adjunctive therapies clearly played a role in disease control in that trial. In the axillary lymph node dissection arm, 27% of patients were found to have additional positive nodes, and we can assume the same would be true in the sentinel node biopsy arm, but after sentinel node biopsy alone, only 0.9% had axillary relapse. All patients received whole-breast irradiation, and at least 96% per arm received systemic treatment. This is important to keep in mind.
Change in Practice
So, which patients still need an axillary dissection, and for whom can it be safely eliminated?
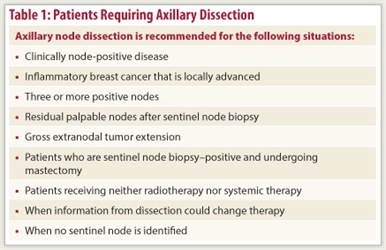
 Sentinel node biopsy can now replace dissection for lumpectomy patients with negative nodes undergoing either lumpectomy or mastectomy. Sentinel node biopsy can also replace dissection for lumpectomy patients with one to two positive sentinel nodes where data on the precise number of additional positive axillary nodes is not needed for treatment decisions. At present, we still recommend axillary lymph node dissection for patients with palpable axillary nodes, three or more positive sentinel nodes, gross extranodal tumor and positive sentinel nodes after neoadjuvant therapy, or when patients undergoing mastectomy have positive nodes (Table 1). We are likely to see trials comparing radiation to dissection in such patients.
Sentinel node biopsy can now replace dissection for lumpectomy patients with negative nodes undergoing either lumpectomy or mastectomy. Sentinel node biopsy can also replace dissection for lumpectomy patients with one to two positive sentinel nodes where data on the precise number of additional positive axillary nodes is not needed for treatment decisions. At present, we still recommend axillary lymph node dissection for patients with palpable axillary nodes, three or more positive sentinel nodes, gross extranodal tumor and positive sentinel nodes after neoadjuvant therapy, or when patients undergoing mastectomy have positive nodes (Table 1). We are likely to see trials comparing radiation to dissection in such patients.
Many of us in practice embrace the Z0011 results and thus reserve axillary dissection for patients not meeting Z0011 criteria and those with gross disease upon palpation. This change in practice is a real quality-of-life advance for our patients. ■
Disclosure: Dr. Smith reported no potential conflicts of interest.
SIDEBAR: International Study Confirms ACOSOG Z0011
References
1. Guiliano AE, Hunt KK, Ballman KV, et al: Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA. 305:569-575, 2011.
2. Krag DN, Anderson SJ, Julian TB, et al: Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: Results from the NSABP B-32 randomized phase III trial. Lancet Oncol 8:881-888, 2007.
3. Mansel RE, Fallowfield L, Kissin M, et al: Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: The ALMANAC trial. J Natl Cancer Inst 98:599-609, 2006.
4. Veronesi U, Paganelli G, Viale G, et al: A randomized comparison of sentinel node biopsy with routine axillary dissection in breast cancer. N Engl J Med 349:546-553, 2003.
5. Fiedler AG, Covarrubias FD, Kim E, et al: Risk of axillary recurrence after a negative sentinel node biopsy without radiation: Implications for partial breast irradiation. 2010 Breast Cancer Symposium. Abstract 22. Presented October 2, 2012.
6. Cote R, Giuliano AE, Hawes D, et al: ACOSOG Z0010: A multicenter prognostic study of sentinel node and bone marrow micrometastases in women with clinical T1/T2 N0M0 breast cancer. J Clin Oncol 28(18S):Abstract CRA504, 2010.
7. Weaver DL, Ashikaga T, Krag DN, et al: Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med 364:412-421, 2011.
8. Galimberti V, Cole BF, Zurrida S, et al: Update of International Breast Cancer Study Group Trial 23-01 to compare axillary dissection versus no axillary dissection in patients with clinically node negative breast cancer and micrometastases in the sentinel node. 2011 San Antonio Breast Cancer Symposium. Abstract S3-1. Presented December 8, 2011.

 Preliminary findings of the International Breast Cancer Study Group (IBCSG) 23-01 trial1 show no benefit for axillary lymph node dissection in patients with only minimally involved sentinel nodes, thereby supporting the results of the American College of Surgeons Oncology Group (ACOSOG) Z0011...
Preliminary findings of the International Breast Cancer Study Group (IBCSG) 23-01 trial1 show no benefit for axillary lymph node dissection in patients with only minimally involved sentinel nodes, thereby supporting the results of the American College of Surgeons Oncology Group (ACOSOG) Z0011...