
Elizabeth Morris, MD
BREAST CANCER SCREENING is no longer “just mammography” but involves a growing list of ever more sophisticated techniques that are improving detection, according to Elizabeth Morris, MD, Professor of Radiology, the Larry Norton Chair, and Chief of the Breast Imaging Service at Memorial Sloan Kettering Cancer Center, New York. At the 2019 Miami Breast Cancer Conference, Dr. Morris described new approaches that are advancing the field of imaging.1
Current mammographic techniques (two-dimensional [2D] film screen or three-dimensional [3D] tomosynthesis) detect cancer at the time of tumor growth, ie, “after the tumor has declared itself.” Newer techniques such as magnetic resonance imaging (MRI) and contrast-enhanced digital mammography can detect cancer a bit earlier by revealing blood vessel growth related to the tumor.
However, optimally, she said, imaging should be able to reveal cancer at an even earlier stage, such as by showing the presence of growth factors spurring the tumor’s growth. “This is where—with very, very early detection—we could have a huge impact on mortality,” she indicated.
Although imperfect, mammographic techniques have improved over time. The currently used tomosynthesis, ie, 3D mammography, offers a higher detection rate and lower recall rate than the older 2D mammography, but it does not eliminate the problem of dense breasts. Even with tomosynthesis, density can obscure cancer on mammography. In fact, women with extremely dense breasts are 17 times more likely to develop interval cancers and should always be further evaluated with ultrasonography. Also, even with the best mammography, screen-detected cancers have become metastatic in 10% of women. “So, mammography works for most women, but not all,” she noted.
“We are moving away from whole population–based [breast cancer] screening to a more individualized screening approach.”— Elizabeth Morris, MD
Tweet this quote
Contrast-Based MRI Advantages
CONTRAST-BASED SCREENING is “potentially a big disrupter in this space,” yielding more accurate diagnoses and time savings for clinicians, Dr. Morris said. Contrast-based imaging detects more biologically relevant cancers (ie, high-grade invasive tumors), whereas conventional mammography misses most relevant disease and picks up more tumors like ductal carcinoma in situ.
The contrast-based approaches include contrast-enhanced digital mammography and MRI. Contrast-enhanced digital mammography can reveal small cancers, even in very dense breasts. It is inexpensive and easily integrated into the clinic. Breast MRI is not new, but it has suffered from some degree of “disillusionment,” she added. This should change greatly with the newer form of “abbreviated MRI,” she predicted, explaining this test can be performed in less than 10 minutes; and less time “in the magnet” translates into a cost savings.
“Abbreviated MRI is not only more patient-friendly and less expensive, but I think we will be using it in a more productive way. This can also be said for contrast-enhanced digital mammography,” she added. “Abbreviated MRI and contrast-enhanced digital mammography offer attractive alternatives to mammography plus ultrasound and perhaps should be used in the general population.”
Rapid, abbreviated MRI protocols have been evaluated by several large groups. For instance, in 443 women, Kuhl et al found that very early but biologically relevant cancers could be detected in an “exceedingly inexpensive” 3-minute examination.2 Dr. Morris and her colleagues validated this “ultra-fast” approach and showed it was highly reproducible.3 Figure 1 shows an MRI scan of a 4-mm invasive lobular cancer.
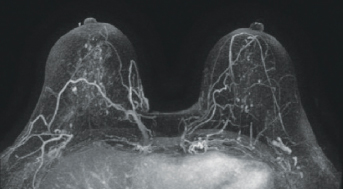
FIGURE 1: An MRI scan of a 4-mm invasive lobular carcinoma.
“This opens the door for a test that can detect very early, small cancers, without an increase in false-positives. It offers improved patient tolerance and competitive pricing,” she said.
Has the Needle Been Moved Enough?
ALTHOUGH THE DETECTION of ever-smaller cancers is laudable, added Dr. Morris, “The question really is, have we moved the point of detection enough? Have the cancers we detect already metastasized? Has clonal expansion already occurred?”
MRI screening does reduce the proportion of advanced-stage cancers, an advantage that is being further evaluated in the ECOG-ACRIN 1141 DENSE trial. The study is comparing abbreviated MRI with 3D tomosynthesis in average-risk women and in women with dense breasts. Although no formal results have been announced, a first look at the data shows that MRI detected twice as many invasive cancers; 3D mammography alone revealed no invasive cancers; and MRI was well tolerated. There are no CPT codes for abbreviated MRI yet, but many practices are offering it for about $300, Dr. Morris has found.
Streamlining Screening
WITH THE BURGEONING USE of genetic profiling in breast cancer, many institutions and trials are performing risk profiling to streamline screening. This risk-adaptive approach often includes the presence of breast cancer–related genes, mammographic density, family history of cancer, lifestyle and hormonal factors, and demographic data.
POSSIBLE ALTERNATIVES TO STANDARD MAMMOGRAPHY
- Magnetic resonance imaging (MRI)
- Abbreviated MRI
- Contrast-enhanced digital mammography
In an international study involving more than 65,000 patients and controls, 77 single nucleotide pleomorphisms, estrogen receptor status, and family history were used to create a polygenic risk score (77-single nucleotide pleomorphisms polygenic risk score).4 The lifetime risks of breast cancer for women in the lowest and highest quintiles of the polygenic risk score were 5.2% and 16.6% for a woman without a family history of breast cancer, respectively, and 8.6% and 24.4% for a woman with a first-degree family history. This level of risk discrimination could inform targeted screening and prevention strategies, Dr. Morris predicted.
“This raises the question of whether American women are ready to leave population-based screening, and it appears they are. They’re very interested in having this sort of personalized approach,” she said. But much works remains to be done. “Genetic risk models and easy-to-perform single nucleotide pleomorphism tests may soon have an impact. I do believe we are moving away from whole population–based screening to a more individualized screening approach.” ■
DISCLOSURE: Dr. Morris has received research support from Komen, Breast Cancer Research Foundation, Grail, GE, Hologic, and Medtronic.
REFERENCES
1. Morris E: The future of screening: Precision vs population? 2019 Miami Breast Cancer Conference. Invited Lecture. Presented March 9, 2019.
2. Kuhl CK, et al: Abbreviated breast magnetic resonance imaging (MRI). J Clin Oncol 32:2304-2310, 2014.
3. Morris EA: Rethinking breast cancer screening: Ultra-FAST breast magnetic resonance imaging. J Clin Oncol 32:2281-2283, 2014.
4. Mavaddat N, Pharoah PD, Michailidou K, et al: Prediction of breast cancer risk based on profiling with common genetic variants. J Natl Cancer Inst 107(5):djv036, 2015.

