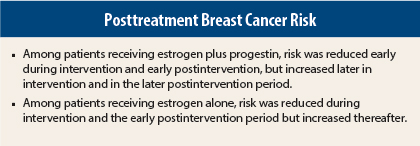
In an analysis of Women’s Health Initiative trials reported in JAMA Oncology, Rowan T. Chlebowski, MD, PhD, of Harbor-UCLA Medical Center, and colleagues found differing patterns of breast cancer risk among women receiving menopausal hormone therapy with estrogen plus progestin or estrogen alone.1 Women receiving estrogen plus progestin had reduced early risk, with risk subsequently increasing throughout treatment and during postintervention follow-up. Women receiving estrogen alone had reduced risk during intervention, which persisted through early postintervention.
Study Details
The study included data from 27,347 postmenopausal women aged 50 to 79 years who were enrolled in two Women’s Health Initiative trials at 40 U.S. centers from 1993 to 1998 and followed for a median of 13 years through September 2010. In one trial,2 16,608 women with a uterus were randomly assigned to estrogen plus progestin (n = 8,506) or placebo (n = 8,102), with a median intervention duration of 5.6 years. In the other, 10,739 women with prior hysterectomy were randomly assigned to estrogen alone (n = 5,310) or placebo (n = 5,429) with a median intervention duration of 7.2 years.3 Annual mammography was protocol mandated and breast cancers were confirmed by medical record review.
Risk in Estrogen/Progestin Trial
In the estrogen-plus-progestin trial, risk of invasive breast cancer was reduced during the first 2 years of intervention (hazard ratio [HR] = 0.71, 95% confidence interval [CI] = 0.47–1.08) due to interference with mammographic detection, but risk increased during the subsequent two 2-year intervals during intervention (HR = 1.36, 95% CI = 0.95–1.94, and HR = 1.65, 95% CI = 1.17–2.32), resulting in a significantly increased risk for the entire intervention period (HR = 1.24, 95% CI = 1.01–1.53) while participants were receiving the combined hormone therapy.
When the therapy was discontinued, the hazard ratio decreased during the early postintervention period. For the entire postintervention period of follow-up, breast cancer risk persisted and was significantly increased (HR = 1.32, 95% CI = 1.08–1.61).
Risk in Estrogen-Alone Trial
In the estrogen-alone trial, risk of invasive breast cancer risk was lower than 1 throughout the intervention period (HR = 0.79, 95% CI = 0.61–1.02). Risk was significantly reduced during the early postintervention period (HR = 0.55, 95% CI = 0.34–0.89) but the effect was attenuated during the late postintervention period (HR = 1.17, 95% CI = 0.73–1.87).
Postintervention Comparisons
In exploratory analyses, characteristics of breast cancers diagnosed during the early vs late postintervention periods differed in both trials, perhaps reflecting the sudden change in estrogen and/or progestin levels. In both trials, however, no differences in patient cancer characteristics were seen comparing intervention to the entire post intervention period.
The investigators concluded: “In the [estrogen-plus-progestin] trial, the higher breast cancer risk seen during intervention was followed by a substantial drop in risk in the early post-intervention phase, but a higher breast cancer risk remained during the late postintervention follow-up. In the estrogen alone trial, the lower breast cancer risk seen during intervention was sustained in the early postintervention phase but was not evident during the late postintervention follow-up.”
They noted: “With longer follow-up of the two Women’s Health Initiative hormone therapy trials, a complex pattern of changing year-to-year influences on breast cancer [risk] was observed. The ongoing influences on breast cancer [risk] after stopping hormone therapy in the Women’s Health Initiative trials require recalibration of breast cancer risk and benefit calculation for both regimens, with greater adverse influence for estrogen and progestin use and somewhat greater benefit for use of estrogen alone.” ■
Disclosure: The Women’s Health Initiative program is supported by the National Heart, Lung, and Blood Institute, National Institutes of Health. For full disclosures of the study authors, visit oncology.jamanetwork.com.
References
1. Chlebowski RT, Rohan TE, Manson JE, et al: Breast cancer after use of estrogen plus progestin and estrogen alone: Analyses of data from two Women’s Health Initiative randomized clinical trials. JAMA Oncol 1:296-305, 2015.
2. Chlebowski RT, Anderson GL, Gass M, et al, WHI Investigators: Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA 304:1684-1692, 2010.
3. Anderson GL, Chlebowski RT, Aragaki A, et al: Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: Extended follow-up of the Women’s Health Initiative randomized placebo-controlled trial. Lancet Oncol 13:476-486, 2012.