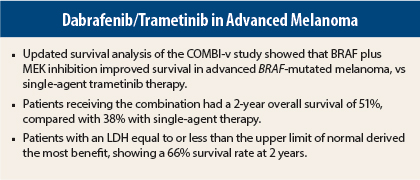
Combined BRAF and MEK inhibition was superior to BRAF inhibition alone in unresectable metastatic melanoma, according to the updated survival analysis of the large randomized COMBI-v trial.1 These findings were reported at the 2015 European Cancer Congress recently held in Vienna, Austria.
“Dabrafenib [Tafinlar] plus trametinib [Mekinist] has demonstrated superiority over BRAF inhibitor monotherapy now in two phase III trials, supporting its use as a standard-of-care therapy in patients with BRAF V600–mutant melanoma,” said lead author Caroline Robert, MD, of Institut Gustave Roussy in Paris.
COMBI-v, which enrolled 704 patients with advanced, treatment-naive BRAF-mutant melanoma, evaluated the BRAF inhibitor dabrafenib plus the MEK inhibitor trametinib and compared it with the single-agent treatment with the first-approved BRAF inhibitor vemurafenib (Zelboraf).
Patients treated with dabrafenib plus trametinib had a 2-year overall survival of 51%, compared with 38% for single-agent vemurafenib treatment.
The updated analysis showed the advantage of combination therapy increases over time. The difference in overall survival has grown from 9% at 1 year, to 10% at 18 months, and to 13% at the 2-year mark, she noted.
COMBI-v is the second trial to show superiority for the combination vs monotherapy in advanced melanoma. It was initiated at the same time as COMBI-d, which showed that overall survival at 2 years was 51%, compared with 42% for single-agent dabrafenib.
These consistent results, Dr. Robert said in a press briefing, “confirm that the combination is superior to BRAF-inhibitor monotherapy…. We can use this treatment as the standard of care for patients with BRAF-mutant melanoma.”
A Closer Look at COMBI-v
In COMBI-v, 704 patients with unresectable, BRAF-mutant, stage III/IV melanoma were randomized to receive the combination of dabrafenib at 150 mg twice daily plus trametinib at 2 mg every day (n = 352) or a standard dose of vemurafenib at 960 mg twice daily
(n = 352). The trial had a primary endpoint of overall survival.
Earlier reports showed a statistically significant improvement in survival at 18 months, from 50% with vemurafenib to 60% with the combination. In the current 2-year analysis, whose data cutoff was March 2015, the absolute difference increased to 13%.
Median overall survival was 25.6 months with combination therapy and 18.0 months with single-agent vemurafenib, a 34% reduction in the hazard ratio (HR = 0.66; P < .001). Median progression-free survival was 12.6 months and 7.3 months, respectively (HR = 0.61; P < .001).
The combination produced more responses (66% vs 53%; P = .0008), including complete responses in 17% of the combination group vs 10% with vemurafenib.
Dr. Robert noted that 98 patients of the combination arm are censored and still on treatment, vs 33 of the vemurafenib arm, which leaves a lot of hope for the follow-up benefit of the combination.
Robust Benefit in Lower LDH Group
Approximately two-thirds of the population had baseline levels of lactate dehydrogenase (LDH)equal to or less than the upper limit of normal. This subset fared particularly well on the combination.
“The longest benefit was in patients with an LDH less than or equal to the upper limit of normal, who had a 2-year overall survival rate of 66% and a median progression-free survival of 17.5 months,” reported Dr. Robert.
In the subgroup of patients with an LDH less than or equal to the upper limit of normal, the median overall survival was not yet reached with the combination and was 21.5 months with vemurafenib (HR = 0.56). Median progression-free survival was 17.5 vs 9.2 months with the combination and monotherapy, respectively, in the low LDH subset (HR = 0.55).
In contrast, patients with an LDH above the upper limit of normal had a median overall survival of 10.6 months with the combination, vs 8.9 months with monotherapy (HR = 0.81), and a median progression-free survival of 5.5 months vs 4.0 months, respectively (HR = 0.70).
These differences were a focus of discussion after her presentation. “Patients with high LDH, whatever treatment we use, remain a big medical need,” Dr. Robert indicated. “They derive a small benefit each time we evaluate a new, effective therapy. The benefit is always less in this population.”
Dr. Robert maintained that high LDH indicates more than tumor burden, rather “something biologic underlies it,” but this remains unclear. “These are interesting hypotheses to explore.”
In contrast, those with low LDH respond extremely well to targeted treatment, she added. “Targeted treatment is very convincing in this group,” she noted.
The combination had a manageable adverse event profile, with no new safety signals with additional 6-month median follow-up. Virtually all patients in each arm experienced an adverse event, but those leading to treatment discontinuation were observed in 16% of the combination arm and in 14% of the vemurafenib arm.
Dr. Robert added that the combination also proved superior in terms of quality of life at all time points, even at progression. ■
Disclosure: Dr. Robert disclosed relevant relationships with Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Merck, Novartis, and Roche. The study was supported by GlaxoSmithKline and Novartis.
Reference
1. Robert C, Karaszewska B, Schachter J, et al: Two year estimate of overall survival in COMBI-v, a randomized, open-label, phase III study comparing the combination of dabrafenib and trametinib vs vemurafenib as first-line therapy in patients with unresectable or metastatic BRAF V600E/K mutation-positive cutaneous melanoma. 2015 European Cancer Congress. Abstract 3301. Presented September 28, 2015.