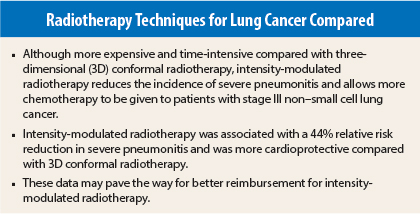
Intensity-modulated radiation therapy appears to be preferable to three-dimensional (3D) conformal radiation therapy as part of treatment for patients with locally advanced (stage III) non–small cell lung cancer (NSCLC). Compared with 3D conformal radiotherapy, intensity-modulated radiotherapy reduced the incidence of severe pneumonitis and allowed more consolidation chemotherapy to be given. Moreover, the low-dose bath with intensity-modulated radiotherapy was not associated with any severe toxicity.
These findings of a secondary analysis of the large randomized NRG Oncology/RTOG 0617 trial, presented at the 2015 American Society for Radiation Oncology (ASTRO) Annual Meeting in San Antonio, Texas, suggest that intensity-modulated radiotherapy should gain a larger role in the treatment of stage III lung cancer.1
“We would advocate that [intensity-modulated radiotherapy] should be routinely considered for stage III lung cancer patients. This study can potentially change practice patterns for locally advanced lung cancer,” said lead author Stephen Chun, MD, Fellow in the Department of Radiation Oncology at The University of Texas MD Anderson Cancer Center, Houston.
Barriers to Adoption
Current National Comprehensive Cancer Network (NCCN®) Clinical Practice Guidelines in Oncology® list both 3D conformal radiotherapy and intensity-modulated radiotherapy techniques as options for management of stage III lung cancers. Intensity-modulated radiotherapy is a more advanced and expensive technique and takes more time for physicians and patients. Planning for this approach is time-intensive, Dr. Chun explained, but it targets radiation to tumor tissue while minimizing exposure to surrounding tissue.
Getting reimbursement for intensity-modulated radiotherapy is a barrier to more widespread adoption. Insurers prefer to reimburse for 3D conformal radiotherapy because it is less expensive. These new data suggest that intensity-modulated radiotherapy can lower the overall costs of treatment by reducing the incidence of severe pneumonitis, which is expensive to treat.
“Our hope is that this study will move along the more widespread adoption of [intensity-modulated radiotherapy] for stage III lung cancer. Perhaps our results might motivate a change in NCCN Guidelines to make [intensity-modulated radiotherapy] the preferred therapy,” Dr. Chun said.
“Cost of hospitalizations for these toxicities is high. If you factor in an absolute 4.5% reduction in grade 3 or higher pneumonitis and multiply that by 70,000 patients per year with stage III NSCLC, the cost savings [with intensity-modulated radiotherapy] could run into billions of dollars,” Dr. Chun told The ASCO Post.
Study Details
NRG Oncology/RTOG 0617 was a large, multi-institutional phase III randomized clinical trial conducted from 2007 to 2011 in patients with locally advanced NSCLC. The original study compared a high dose of radiation (74 Gy) to a standard dose (60 Gy). Patients received concurrent chemotherapy with carboplatin/paclitaxel with or without cetuximab (Erbitux).
The secondary analysis that Dr. Chun presented at the ASTRO Annual Meeting focused on the comparison of intensity-modulated radiotherapy vs 3D conformal radiotherapy. Physicians were allowed to choose radiation technique; of the 482 patients treated with radiotherapy, 47% received intensity-modulated radiotherapy and 53% received 3D conformal radiotherapy, which mirrors practice patterns in the United States, he said.
The original trial did not randomize for radiation technique, so the intensity-modulated radiotherapy group had patients with larger and more advanced-stage tumors considered more difficult to treat; in fact, 38.6% of the intensity-modulated radiotherapy group had stage IIIB tumors vs 30.3% of the 3D conformal radiotherapy group.
Reduced Toxicity
Despite having more advanced tumors, intensity-modulated radiotherapy–treated patients had a lower incidence of grade 3 or higher pneumonitis: 3.5% vs 8% with 3D conformal radiotherapy (P = .046). The protective effect of intensity-modulated radiotherapy was seen in a multivariate analysis and was particularly pronounced in larger tumors, Dr. Chun said.
Although the low-dose bath with intensity-modulated radiotherapy was a concern originally, it was not associated with severe pneumonitis or any other severe toxicity, Dr. Chun pointed out.
Use of intensity-modulated radiotherapy allowed lower doses of radiation to be delivered to the heart, which was associated with improved survival, he said. Intensity-modulated radiotherapy also allowed more consolidative chemotherapy to be administered compared with 3D conformal radiotherapy (37.3% of the intensity-modulated radiotherapy group received full consolidative therapy vs 29.1% of the 3D conformal radiotherapy group).
“We looked at one of the largest clinical trials ever done for NSCLC and found that the most important predictors of severe pneumonitis were intensity-modulated radiotherapy technique and lung V20 [the percentage of lung volume (subtracting the volume involved by lung cancer) that receives radiation doses of 20 Gy or more]. The low-dose bath created by intensity-modulated radiotherapy was not associated with any survival or toxicity outcome. These findings may fundamentally change the way we deliver radiation therapy for locally advanced lung cancer,” Dr. Chun stated. ■
Disclosures: Dr. Chun reported no potential conflicts of interest.
Reference
1. Chun SG, Hu C, Choy H, et al: Comparison of 3-D conformal and intensity modulated radiation therapy outcomes for locally advanced non-small cell lung cancer in NRG Oncology/RTOG 0617. 2015 ASTRO Annual Meeting. Abstract 2. Presented October 18, 2015.