The phase III National Surgical Adjuvant Breast and Bowel Project (NSABP) B-40 (NRG Oncology) trial showed that the addition of bevacizumab (Avastin) to docetaxel + anthracycline-based neoadjuvant chemotherapy improved pathologic complete response rate, the primary endpoint, in patients with early HER2-negative breast cancer; the effect appeared to be greatest in women with hormone receptor–positive tumors.1
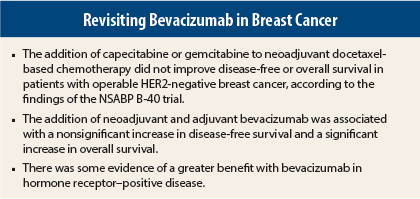
In a report of secondary outcomes in The Lancet Oncology, Harry D. Bear, MD, PhD, of Virginia Commonwealth University School of Medicine and the Massey Cancer Center, Richmond, Virginia, and colleagues found a nonsignificant increase in disease-free survival and a significant increase in overall survival with the addition of neoadjuvant plus adjuvant bevacizumab, with some evidence of greater benefit in hormone receptor–positive disease.2 The addition of capecitabine or gemcitabine to neoadjuvant chemotherapy did not improve disease-free or overall survival.
Study Details
In the 3 × 2 factorial trial, 1,206 patients with clinical stage T1c–3, cN0, cN1, or cN2a disease without distant metastases were randomized between January 2007 and June 2010 to receive 4 cycles of neoadjuvant docetaxel alone (100 mg/m²), with capecitabine (825 mg/m² orally twice daily on days 1–14, docetaxel 75 mg/m²) or with gemcitabine (1,000 mg/m² on days 1 and 8, docetaxel 75 mg/m²). All patients then were given neoadjuvant doxorubicin and cyclophosphamide (60 mg/m² and 600 mg/m²) every 3 weeks for 4 cycles. In addition, all patients were randomized to receive or not receive neoadjuvant bevacizumab (15 mg/kg every 3 weeks for the first 6 neoadjuvant cycles) and postoperative bevacizumab for 10 doses.
Disease-free survival was a prespecified secondary endpoint; although overall survival was not, it was prospectively followed. Follow-up data were collected between October 2007 and March 2014 and were available for overall survival in 1,186 patients and for disease-free survival in 1,184 patients (591 with and 593 without bevacizumab).
Disease-Free and Overall Survival
Median follow-up was 4.7 years. No significant differences between docetaxel alone vs with capecitabine or gemcitabine were observed in 5-year disease-free survival (hazard ratios [HRs = 1.01, 95% confidence interval [CI] = 0.77–1.33, and 0.90, 95% CI = 0.67–1.19) or 5-year overall survival (HRs = 0.95, 95% CI = 0.68–1.32, and 0.73, 95% CI = 0.51–1.04).
The addition of bevacizumab was associated with a borderline increase in disease-free survival (HR = 0.80, 95% CI = 0.63–1.01, P = .06) and a significant increase in overall survival (HR = 0.65, 95% CI = 0.49–0.88, P = .004). Kaplan-Meier analysis showed increasing separation of the curves between bevacizumab and no bevacizumab starting at 2 years for both disease-free and overall survival.
An exploratory analysis suggested a somewhat greater benefit of bevacizumab among patients with hormone receptor–positive tumors (HR = 0.73, P = .05, for disease-free survival; HR = 0.63, P = .03 for overall survival), but the interaction between hormone receptor status and bevacizumab effect was not significant for either outcome. An exploratory analysis of distant recurrence-free interval also showed that the addition of bevacizumab significantly decreased the risk of distant metastasis overall (HR = 0.70, P = .01) and among patients with hormone receptor–positive disease (HR = 0.68, P = .03).
The effect of bevacizumab was greater in the groups in which patients received gemcitabine or capecitabine with docetaxel. The interaction between the effect of bevacizumab and the treatment group was significant for distant recurrence-free interval but not for disease-free survival or overall survival.
Toxicity
The most common grade 3 or 4 adverse events in the bevacizumab group were neutropenia (17% grade 3, 6% grade 4), hand-foot syndrome (11% grade 3), and hypertension (10% grade 3, < 1% grade 4). The most common grade 3 or 4 adverse events in the no-bevacizumab group were neutropenia (16% grade 3, 6% grade 4), fatigue (9% grade 3), and hand-foot syndrome (7% grade 3). Four deaths occurred during treatment, due to vascular disorder (docetaxel-capecitabine group), sudden death (docetaxel-capecitabine group), infective endocarditis (docetaxel plus bevacizumab group), and visceral arterial ischemia (docetaxel group).
The investigators concluded: “The addition of gemcitabine or capecitabine to neoadjuvant docetaxel plus doxorubicin plus cyclophosphamide does not seem to provide any benefit to patients with operable breast cancer and should not change clinical practice in the short term. The improved overall survival with bevacizumab contradicts the findings of other studies of bevacizumab in breast cancer and may indicate the need for additional investigation of this agent.”
They noted: “The pattern of the bevacizumab effect seen here, with the greatest effect being on distant metastases and being proportionately greater beyond 2 years of follow-up, also suggests a predominant effect on occult micrometastases present at the time of diagnosis. This also fits with the preferential effect of bevacizumab in women with hormone-receptor-positive cancers, whose recurrences tend to be later than for patients with triple-negative breast cancer.” ■
Disclosure: The study was funded by the National Institutes of Health, Genentech, Roche Laboratories, Lilly Research Laboratories, and Precision Therapeutics. For full disclosures of the study authors, visit www.thelancet.com.
References
1. Bear HD, Tang G, Rastogi P, et al: Bevacizumab added to neoadjuvant chemotherapy for breast cancer. N Engl J Med 366:310-320, 2012.
2. Bear HD, Tang G, Rastogi P, et al: Neoadjuvant plus adjuvant bevacizumab in early breast cancer (NSABP B-40 [NRG Oncology]): Secondary outcomes of a phase 3, randomised controlled trial. Lancet Oncol 16:1037-1048, 2015.