The 2011 Breast Cancer Symposium was recently held in San Francisco, bringing together a multidisciplinary group of specialists and sponsored by ASCO, the American Society for Radiation Oncology, the Society of Surgical Oncology, the American Society of Breast Disease, the American Society of Breast Surgeons, and the National Consortium of Breast Centers, Inc. The following reports are brief summaries of a few noteworthy presentations.
Irradiating Internal Mammary Nodes
 The value of irradiating the internal mammary nodes continues to be debated. This analysis from the British Columbia Cancer Agency in Vancouver found that intentional inclusion of the internal mammary node region did not result in a significant difference in survival, though a small and nonsignificant 3% survival benefit was observed in the subset with one to three positive nodes.1
The value of irradiating the internal mammary nodes continues to be debated. This analysis from the British Columbia Cancer Agency in Vancouver found that intentional inclusion of the internal mammary node region did not result in a significant difference in survival, though a small and nonsignificant 3% survival benefit was observed in the subset with one to three positive nodes.1
The study included 2,413 women with early breast cancer who received locoregional radiotherapy and were evaluated according to whether this treatment included internal mammary nodes (n = 1,000) or not (n = 1,413). At a median follow-up of 6.2 years, 5-year recurrence-free survival was 81% and 82%, respectively; distant recurrence-free survival was 82% per arm, and overall survival was 85% and 83% (no statistically significant differences). In the subset with one to three positive nodes, overall survival was 91% for patients who received radiotherapy to the internal mammary nodes and 88% for those who did not—a 22% nonsignificant risk reduction.
“Women with low-burden, node-positive disease are most likely to benefit from internal mammary node radiotherapy,” said Robert Olson, MD, who presented the findings.
Barbara Fowble, MD, of the University of California School of Medicine, San Francisco, the formal discussant of the study, said she sees “problems with the data, but recognizing this, the study suggests there is no benefit.” The 3% overall survival benefit in node-positive patients is not necessarily a result of the internal mammary node radiotherapy, Dr. Fowble pointed out.
After controlling for potentially confounding factors including age, stage, grade, histology, lymphovascular invasion, ER status, type of surgery, and systemic therapy, there was no significant benefit to intentional inclusion of the internal mammary nodal region (HR = 0.95; 95% CI = 0.78–1.15; P = .57). Within the subset of patients with one to three positive nodes, women who received internal mammary nodal radiotherapy had a nonsignificantly better overall survival than women who did not (HR = 0.78; 95% CI = 0.56–1.09; P = .18).
She added that while toxicity data were not presented, there are “clues” from other analyses that internal mammary node radiotherapy will contribute to toxicity. In her own practice, Dr. Fowble utilizes internal mammary node radiotherapy only when patients are known to have positive internal mammary nodes.
Study Describes Clinical Presentation of Breast Cancer
The importance of annual screening mammography, not only in women older than 50 years but also in women aged 40 to 49, was evaluated in an analysis of a statewide breast cancer registry of 5,903 Michigan women.3 Mammography detected 65% of the breast cancers. Women younger than 50 accounted for 26% of all breast cancers and were equally likely to have had their cancer found by mammography as by clinical exam or breast self-exam (46% and 54%, respectively). When compared with patients with mammographically detected tumors, patients who presented with palpable masses presented at later stages (50% stage II vs 18%) and were more likely to receive chemotherapy (22.7% vs 15.7%) and mastectomies (45.8% vs 27.1%).

 The United States Preventive Services Task Force (USPSTF) recommended in 2009 against routine screening before age 50 and against teaching breast self-exam at any age, and maintained that the evidence on clinical breast exam was insufficient. According to these recommendations, 42% of the Michigan cohort may have been affected by these proposed screening recommendations.
The United States Preventive Services Task Force (USPSTF) recommended in 2009 against routine screening before age 50 and against teaching breast self-exam at any age, and maintained that the evidence on clinical breast exam was insufficient. According to these recommendations, 42% of the Michigan cohort may have been affected by these proposed screening recommendations.
At a press briefing, Jamie Caughran, MD, of the Lacks Cancer Center in Grand Rapids, Michigan, declined to say whether the study contradicts the USPSTF guidelines, but offered, “You are less likely to need chemotherapy [with mammographically detected tumors], so we would support the rest of the societies that continue to recommend annual screening mammography starting at age 40,” because registry population was that of women who had a diagnosis of breast cancer, unlike USPSTF guidelines that examine a screening population.
Andrew Seidman, MD, of Memorial Sloan-Kettering Cancer Center, who moderated the press briefing, said that while debate will continue, this study speaks to another important consequence of screening: reduced need for chemotherapy. “This is a very important gain, independent of any potential survival benefit,” he said.
Nomogram Predicts for Lymphedema
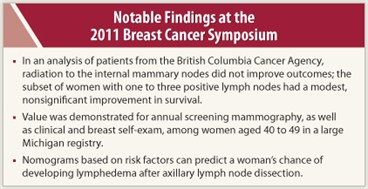 A new set of nomograms based on risk factors can predict a woman’s chance of developing lymphedema after axillary lymph node dissection, Brazilian investigators reported.4 The researchers followed 1,054 patients with breast cancer who had axillary lymph node dissection, evaluating the occurrence of lymphedema according to several risk factors. They developed three possible models that could be used at different time points (preoperatively, within 6 months of surgery, and 6 months or more postoperatively). The models incorporated age, body mass index, number of neoadjuvant and adjuvant chemotherapy infusions, extent of axillary lymph node dissection, location of radiation therapy field, and the development of postoperative seroma and early edema.
A new set of nomograms based on risk factors can predict a woman’s chance of developing lymphedema after axillary lymph node dissection, Brazilian investigators reported.4 The researchers followed 1,054 patients with breast cancer who had axillary lymph node dissection, evaluating the occurrence of lymphedema according to several risk factors. They developed three possible models that could be used at different time points (preoperatively, within 6 months of surgery, and 6 months or more postoperatively). The models incorporated age, body mass index, number of neoadjuvant and adjuvant chemotherapy infusions, extent of axillary lymph node dissection, location of radiation therapy field, and the development of postoperative seroma and early edema.
Within 5 years of axillary lymph node dissection, 30.3% of the women developed lymphedema. All the risk factors in the model were significantly associated with the occurrence of lymphedema and were accurate 70% to 74% of the time. The investigators have converted the models into free, user-friendly calculators that will become public once their results are published. ■
Disclosure: Drs. Olson, Fowble, Caughran, and Seidman reported no potential conflicts of interest.
References
1. Olson RA, Woods R, Lau J, et al: Impact of internal mammary node inclusion in the radiation treatment volume on the outcomes of patients with breast cancer treated with locoregional radiation after six years of follow-up. 2011 Breast Cancer Symposium. Abstract 81. Presented September 8, 2011.
2. Revesz E, Zalles CM, Ivancic D, et al: Relationship of recent pregnancy and cytologic atypia in the contralateral breast of patients with breast cancer. 2011 Breast Cancer Symposium. Abstract 149. Presented September 9, 2011.
3. Smith DR, Caughran J, Kreinbrink JL, et al: Clinical presentation of breast cancer: Age, stage, and treatment modalities in a contemporary cohort of Michigan women. 2011 Breast Cancer Symposium. Abstract 1. Presented September 8, 2011.
4. Bevilacqua JB, Kattan MW, Yu C, et al: Nomograms for predicting the risk of arm lymphedema after axillary dissection in breast cancer. 2011 Breast Cancer Symposium. Abstract 8. Presented September 8, 2011.

