In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
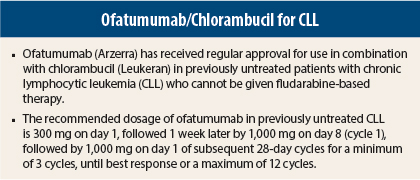
On April 17, 2014, ofatumumab (Arzerra) received regular approval for use in combination with chlorambucil (Leukeran) in previously untreated patients with chronic lymphocytic leukemia (CLL) for whom fludarabine-based therapy is considered inappropriate.1,2 Ofatumumab was granted accelerated approval for use in CLL refractory to fludarabine and alemtuzumab (Campath) in 2009.
Pivotal Study
Approval was based on an open-label trial in which 447 patients for whom fludarabine-based therapy was considered inappropriate by investigators (eg, due to advanced age or comorbidities) were randomly assigned to receive ofatumumab/chlorambucil (n = 217) or chlorambucil alone (n = 227). Ofatumumab was given as an infusion at 300 mg on day 1 of cycle 1, 1,000 mg on day 8 of cycle 1, and 1,000 mg on day 1 of all subsequent 28-day cycles. Chlorambucil was given at 10 mg/m2 orally on days 1 to 7 every 28 days. Prior to each infusion of ofatumumab, patients received premedication with acetaminophen, an antihistamine, and a glucocorticoid.
Overall, patients had median age of 69 years, with 69% of patients in both groups aged ≥ 65 years, 63% were male, 89% were white, 72% had at least two comorbidities, 48% had creatinine clearance < 70 mL/min, and 72% had beta-2 microglobulin levels > 3,500 µg/L.
Median progression-free survival, the primary endpoint, was 22.4 months in the ofatumumab/chlorambucil group vs 13.1 months in the chlorambucil group (hazard ratio [HR] = 0.57, P < .001). Objective response occurred in 82.4% (complete response in 12%) vs 68.6% (complete response in 1%) of patients (P = .001), and median duration of response was 22.1 vs 13.2 months.
How It Works
Ofatumumab is a CD20-directed cytolytic monoclonal antibody that binds specifically to both the small and large extracellular loops of the CD20 402 molecule. The CD20 molecule is expressed on normal B lymphocytes (pre-B to mature B lymphocytes) and on B-cell CLL and is neither shed from the cell surface nor internalized following antibody binding.
The Fab domain of ofatumumab binds to the CD20 molecule and the Fc domain mediates immune effector functions, resulting in B-cell lysis in vitro. The potential mechanisms of cell lysis include complement-dependent cytotoxicity and antibody-dependent cell-mediated cytotoxicity.
How It Is Given
The recommended dosage of ofatumumab in previously untreated CLL is 300 mg on day 1 (at an initial infusion rate of 12 mL/h) followed 1 week later by 1,000 mg (25 mL/h) on day 8 (cycle 1), followed by 1,000 mg (25 mL/h) on day 1 of subsequent 28-day cycles for a minimum of 3 cycles and until best response or a maximum of 12 cycles.
Patients should receive premedication with oral acetaminophen at 1,000 mg (or equivalent), oral or intravenous antihistamine (diphenhydramine at 50 mg or cetirizine at 10 mg or equivalent), and intravenous corticosteroid (prednisolone at 50 mg or equivalent) 30 minutes to 2 hours prior to each infusion.
In the absence of an infusion-related reaction, the rate of infusion can be increased at 30-minute intervals to 25, 50, 100, 200, and 400 mL/h for the day 1, cycle 1 dose and to 50, 100, 200, and 400 mL/h for other doses. Infusion should be interrupted for reactions of any severity.
If the reaction resolves or remains no higher than grade 2, treatment can be resumed at half the previous infusion rate after grade 1 or 2 reactions and at 12 mL/h after grade 3 or 4 reactions. Permanent discontinuation should be considered if severity of the infusion reaction does not resolve to grade 2 or lower despite adequate clinical intervention.
Safety Profile
In the randomized trial, the most common clinical adverse events of any grade in the ofatumumab/chlorambucil group were infusion reactions (67% vs 0% in chlorambucil group), neutropenia (27% vs 18%), asthenia (8% vs 5%), headache (7% vs 3%), leukopenia (6% vs 2%), and herpes simplex (6% vs 4%). The most common grade 3 or 4 adverse events were neutropenia (26% vs 14%), infusion reactions (10% vs 0%), and leukopenia (3% vs < 1%). Grade 3 or 4 hematologic abnormalities consisted of neutropenia in 29% vs 24%, lymphopenia in 29% vs 7%, and leukopenia in 23% vs 4%.
Ofatumumab carries boxed warnings for hepatitis B virus reactivation, which has resulted in fulminant hepatitis, hepatic failure, and death in some cases, and for progressive multifocal leukoencephalopathy resulting in death.
Ofatumumab also has warnings/precautions for infusion reactions, tumor lysis syndrome, and cytopenias. Tumor lysis syndrome should be anticipated in high-risk patients, and premedication with antihyperuricemic agents and hydration should be performed. Late-onset and prolonged neutropenia have been observed. Complete blood counts should be monitored at regular intervals. ■
References
1. U.S. Food and Drug Administration: Ofatumumab. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm393823.htm.
2. ARZERRA® (ofatumumab) injection prescribing information. GlaxoSmithKline, April 2014. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2014/125326s060lbl.pdf.