Patients with early-stage breast cancer who underwent sentinel lymph node dissection experienced lymphedema with increasing incidence over time, according to a presentation at the 2014 Society of Surgical Oncology (SSO) Cancer Symposium in Phoenix.1
In women who took part in the American College of Surgeons Oncology Group (ACOSOG) Z0010 trial, the cumulative incidence of lymphedema after sentinel lymph node dissection was 10.5% at 1 year, 17.4% at 3 years, and 24.1% at 5 years based on objective measurements, reported Mediget
Teshome, MD, of The University of Texas MD Anderson Cancer Center in Houston, and colleagues. Based on subjective assessments, the cumulative incidence of lymphedema was 3.7% at 1 year, 8.9% at 3 years, and 11.9% at 5 years.
Sentinel lymph node dissection is a minimally invasive approach to axillary staging in early-stage breast cancer, and “when compared to traditional axillary lymph node dissection, many studies have demonstrated decreased morbidity with this approach,” Dr. Teshome said during her presentation at an SSO Plenary Session.
However, a potential complication of sentinel lymph node dissection is lymphedema, and long-term studies on this outcome have been lacking, she explained.
The results of ACOSOG Z0010, which was conducted from 1999 to 2003, showed no difference in overall survival, locoregional recurrence, or distant metastasis in patients with occult sentinel lymph node micrometastases by immunohistochemistry.2,3
Current Study
For the current follow-up study, eligible patients were women from ACOSOG Z0010 with clinical T1-2, N0, M0 disease. Of eligibile patients, 4,865 women underwent arm measurement assessment at baseline and at least one other time point. All underwent sentinel lymph node dissection, with 3,966 in the sentinel lymph node dissection–only group and 899 who underwent completion axillary lymph node dissection. The vast majority of women underwent whole-breast irradiation (89.7%), more than half received chemotherapy (56.5%), and about two-thirds had hormonal therapy (66.9%).
Lymphedema was evaluated objectively as an increase of 2 cm from the preoperative arm measurement vs the contralateral arm, corresponding with a 10% increase in arm volume, Dr. Teshome said. Subjective measurement consisted of ipsilateral arm swelling as reported by the patient.
Assessments were performed before sentinel lymph node dissection and then again at 30 days, 6 months, and annually for 5 years after surgery. The median number of assessments was four, and the median follow-up time was 9.9 years, although arm measurements were only done to 5 years.
Dr. Teshome pointed out that there was attrition of arm measurements over time, with 69.9% of women undergoing assessment at 1 year, 51.5% at 3 years, and 27.6% at 5 years, but the authors were still able to analyze data in over 1,000 patients.
Outcomes
In the sentinel lymph node dissection–only group who experienced lymphedema, the authors found that patients were older (age 58 vs 56, P < .0001), had a body mass index of 30 kg/m2 and higher (40.9% vs 25.5%, P < .0001), and had a lower percentage of medially located tumors (17.2% vs 21.2%, P = .016).
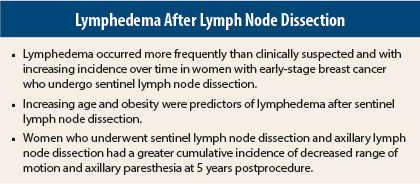
Although the authors reported that lymphedema after sentinel lymph node dissection “occurs more frequently than clinically suspected and with increasing incidence over time,” they also noted that women who had only sentinel lymph node dissection fared better than those who required axillary lymph node dissection.
When comparing the two techniques, the 5-year incidence rate by subjective assessment was 41.2% for axillary lymph node dissection compared with 11.9% for sentinel lymph node dissection, while the 5-year incidence rate by objective assessment was 40.3% vs 24.1%. This is compared to the prevalance of lymphedema after sentinel lymph node dissection at each measurement point, which varied from 6.5% to 9.2% for objective assessment and 2.1% to 3.7% for subjective assessment.
Additionally, patients undergoing axillary lymph node dissection had a greater cumulative incidence of decreased range of motion and axillary paresthesia at 5 years (51.3% and 76.3%, respectively) compared with sentinel lymph node dissection patients (22.1% and 29.1%).
Both increasing age (hazard ratio [HR] = 1.01, 95% confidence interval [CI] = 1.01–l.02, P < .003) and obesity (HR = 1.89, 95% CI = 1.61–2.22, P < .0001) were predictors of lymphedema after sentinel lymph node dissection. However, increasing age, presence of axillary seroma, and African American race were predictors of decreased range of motion and axillary paresthesia following axillary lymph node dissection.
Study Discrepancies and Limitations
Dr. Teshome called attention to some “notable and interesting points” in the study results.
“First, as expected, there is an increased incidence of lymphedema after axillary lymph node dissection as compared to sentinel lymph node dissection,” she said. “Second, looking specifically at women undergoing sentinel lymph node dissection, there appears to be a plateau effect over time with regard to the subjective determination of lymphedema, while the cumulative incidence by objective arm measurements seems to slowly increase over time. Lastly, there is discrepancy between the subjective and objective reports of lymphedema, with approximately twice as many cases by objective measures.”
But the latter was not true in the axillary lymph node dissection group, where cumulative subjective and objective data were essentially the same, she said. She added that the discrepancy in patients undergoing sentinel lymph node dissection may be explained by improvement in lymphedema symptoms over time secondary to interventions.
That said, there was limited follow-up on lymphedema treatment or symptom improvement, Dr. Teshome noted. Other limitations were the lack of randomization, and attrition in arm measurements during the study period, which meant that every patient did not have a complete assessment profile.
“Lastly, the majority of our patients received radiation therapy, and although there was no association in our analysis, this may have impacted the findings,” she said.
Dr. Teshome said future areas of research would include the evaluation of severity of lymphedema after sentinel lymph node dissection, assessment of patient education on post–sentinel lymph node dissection symptoms, and lymphedema prevention efforts. ■
Disclosure: This study was funded by the National Cancer Institute. Dr. Teshome reported no potential conflicts of interest.
References
1. Teshome M, Ballman KV, McCall LM, et al: Long-term incidence of lymphedema after sentinel lymph node dissection for early stage breast cancer: ACOSOG Z0010 (Alliance). 2014 SSO Cancer Symposium. Abstract 3. Presented March 14, 2014.
2. Giuliano AE, Hunt KK, Ballman KV, et al: Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: A randomized clinical trial. JAMA 305:569-575, 2011.
3. Hunt KK, Ballman KV, McCall LM, et al: Factors associate with local-regional recurrence after a negative sentinel lymph node dissection: Results of the ACOSOG Z0010 trial. Ann Surg 256:428-436, 2012.