
The ASCO Post’s Integrative Oncology series is intended to facilitate the availability of evidence-based information on integrative and complementary therapies commonly used by patients with cancer. In this installment, Ting Bao, MD, DABMA, MS, reviews the current data on the use of acupuncture for managing chemotherapy-induced peripheral neuropathy and suggests further randomized controlled trials with larger sample sizes, placebo controls, and objective endpoints are needed.
Chemotherapy-induced peripheral neuropathy is an adverse event commonly associated with anticancer agents, including taxanes, platinums, vinca alkaloids, bortezomib (Velcade), and thalidomide (Thalomid).1,2 Symptoms such as pain, numbness, tingling, and autonomic neuropathy produce significant negative effects on quality of life that can continue for years.3,4
Joint American Cancer Society (ACS)-ASCO Guidelines5,6 recommend duloxetine for patients with neuropathic pain (level of evidence, IB) based on one randomized double-blind placebo-controlled crossover trial.7 However, previous guidelines8 concluded that data provided only moderate support for its use. Furthermore, among 42 randomized controlled trials of 19 interventions evaluated for the prevention of chemotherapy-induced peripheral neuropathy, none were effective, and some even caused harm,8 highlighting a critical need for additional approaches.
Viewed by many patients as a natural alternative to medicine,9 acupuncture is among the nonpharmacologic interventions already recommended for patients with cancer to address pain (level of evidence, I), including aromatase inhibitor–associated arthralgia and musculoskeletal health (level of evidence, III).5,6,10,11 In addition, preliminary studies suggest benefits with acupuncture for peripheral neuropathy,12 including peripheral neuropathy associated with diabetes,13 acquired immune deficiency syndrome,14,15 or chemotherapy.16-18 Therefore, acupuncture is worthy of further study for this purpose.
Current Evidence
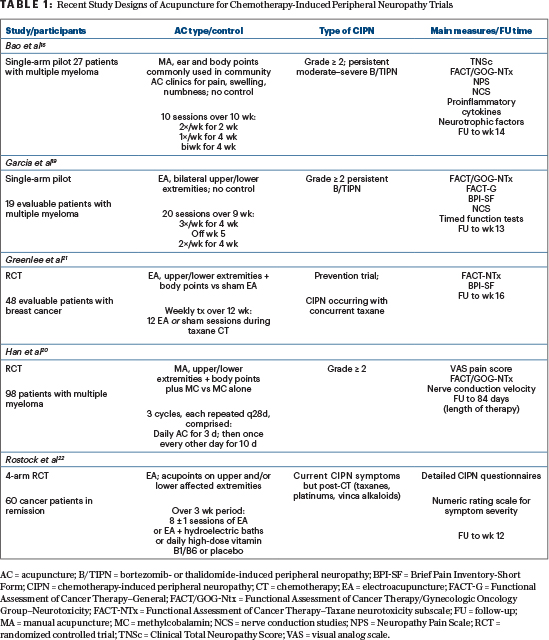
Two single-arm pilot studies16,19 (see Table 1 on page 80) evaluated different types of acupuncture for patients with multiple myeloma who experienced persistent bortezomib- and/or thalidomide-induced peripheral neuropathy. In our study (N = 27),16 manual acupuncture significantly improved moderate-to--severe bortezomib-induced peripheral neuropathy pain at 10-week treatment completion and 4 weeks postintervention (both P < .0001). In addition, compliance was high (> 90%), with no safety issues reported.

Ting Bao, MD, DABMA, MS
In the study by Garcia et al,19 electroacupuncture significantly improved bortezomib- and/or thalidomide-induced peripheral neuropathy in 19 evaluable patients (≥ 80% of sessions received). Benefits began at week 4, with the largest effect at 9-week treatment completion and sustained improvements at 13 weeks (P = .0002). Timed-function test scores also significantly improved (P ranges from .02 to < .0001).
In a subsequent randomized controlled trial of manual acupuncture along with methylcobalamin among 98 patients with multiple myeloma, the combination regimen was significantly better than methylcobalamin alone, as measured by visual analogue scale pain scores (P < .01), Functional Assessment of Cancer Therapy/Gynecologic Oncology Group–Neurotoxicity (P < .001), and nerve conduction velocity studies (P ranges from < .05 to < .01).20
In contrast, two randomized controlled trials of electroacupuncture have yielded negative study results. In a chemotherapy-induced peripheral neuropathy prevention trial by Greenlee et al21 among 48 evaluable patients with breast cancer who received either electroacupuncture or sham treatment during taxane chemotherapy for 12 weeks, no between-group differences were observed at treatment completion. In addition, those receiving electroacupuncture actually had worse symptoms at week 16, with a longer pain-recovery time. The focus on chemotherapy-induced peripheral neuropathy prevention rather than treatment along with the use of electrical rather than manual forms of acupuncture raises questions about the context in which these regimens may be effective.
In a 4-arm study by Rostock et al (N = 60),22 there were no significant differences in improvements among patients randomized to receive electroacupuncture, electroacupuncture with hydroelectric baths, high-dose vitamin B1/B6, or placebo. Here, investigators cite baseline low-level intensity of chemotherapy-induced peripheral neuropathy complaints, especially in the electroacupuncture group, and sample size calculations that were based on patients having more severe symptoms.
Design Challenges and Safety Concerns
Two pilot studies and one randomized controlled trial have established that both manual acupuncture and electroacupuncture can be safe and feasible for the treatment of chemotherapy-induced peripheral neuropathy, but two negative randomized controlled trials with electroacupuncture (one a prevention study) raises questions about different effects across acupuncture modalities, utility, and timing. Mechanisms by which acupuncture may elicit improvements remain unclear. Preliminary evidence points to proinflammatory cytokine
ACS/ASCO SURVIVORSHIP CARE GUIDELINE: LEVEL OF EVIDENCE
- 0 Expert opinion, observational study (excluding case-control and prospective cohort studies), clinical practice, literature review, or pilot study
- I Meta-analyses of randomized controlled trials
- IA Randomized controlled trial of breast cancer survivors
- IB Randomized controlled trial based on cancer survivors across multiple cancer sites
- IC Randomized controlled trial not based on cancer survivors but on the general population experiencing a specific long-term or late effect
- IIA Nonrandomized clinical trials based on breast cancer survivors
- IIB Nonrandomized clinical trials based on cancer survivors across multiple cancer sites
- IIC Nonrandomized clinical trials not based on cancer survivors but on the general population experiencing a specific long-term or late effect
- III Case-control study or prospective cohort study
inhibition23 or central nervous system effects caused by the dynamics between afferent impulses from pain regions and impulses from stimulated acupoints.24 However, nerve conduction improvements were not observed in the previously mentioned pilots16,19 as with other studies,20,25 nor were there any effects on proinflammatory or neurotrophic cytokine levels, although disease status and treatment may make such detection difficult.16 And even with no apparent differences between sham acupuncture and electroacupuncture in both randomized controlled trials, whether sham acupuncture can be made completely inert remains an open question.25,26 In addition, increased stimulation with electroacupuncture over manual acupuncture may not always translate to “more is better,” and effective regimens may differ for prevention versus treatment. Here are just some of the difficulties associated with study design and interpreting results to further elucidate acupuncture type, dosing, and mechanisms.
Future Directions
The current evidence is promising but warrants further randomized controlled trials with larger sample sizes, placebo controls, and objective endpoints such as nerve conduction studies or quantitative sensory testing. Additional studies on the mechanisms by which acupuncture helps reduce symptoms of chemotherapy-induced peripheral neuropathy are also needed. Furthermore, assessing changes in cytokines and neurotrophic factors may be worthwhile. In addition, functional magnetic resonance imaging previously used to evaluate acupuncture for other types of neuropathic pain may help bridge the mechanism-effects gap for acupuncture in chemotherapy-induced peripheral neuropathy.27
Acknowledgement: Dr. Bao would like to thank Ingrid Haviland, Assistant Editor at the Memorial Sloan Kettering Cancer Center’s Integrative Medicine Service, for her writing and editorial assistance. ■
Dr. Bao is Director, Integrative Breast Oncology, Integrative & Breast Medicine Services, Memorial Sloan Kettering Cancer Center, New York.
DISCLOSURE: Dr. Bao reported no conflicts of interest.
REFERENCES
1. Bao T, Basal C, Seluzicki C, et al: Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: Prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159:327-333, 2016.
2. Park SB, Goldstein D, Krishnan AV, et al: Chemotherapy-induced peripheral neurotoxicity: A critical analysis. CA Cancer J Clin 63:419-437, 2013.
3. Kidwell KM, Yothers G, Ganz PA, et al: Long-term neurotoxicity effects of oxaliplatin added to fluorouracil and leucovorin as adjuvant therapy for colon cancer: Results from National Surgical Adjuvant Breast and Bowel Project trials C-07 and LTS-01. Cancer 118:5614-5622, 2012.
4. Hershman DL, Weimer LH, Wang A, et al: Association between patient reported outcomes and quantitative sensory tests for measuring long-term neurotoxicity in breast cancer survivors treated with adjuvant paclitaxel chemotherapy. Breast Cancer Res Treat 125:767-774, 2011.
5. Runowicz CD, Leach CR, Henry NL, et al: American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J Clin Oncol 34:611-635, 2016.
6. Runowicz CD, Leach CR, Henry NL, et al: American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J Clin 66:43-73, 2016.
7. Smith EM, Pang H, Cirrincione C, et al: Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: A randomized clinical trial. JAMA 309:1359-1367, 2013.
8. Hershman DL, Lacchetti C, Dworkin RH, et al: Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 32:1941-1967, 2014.
9. Mao JJ, Leed R, Bowman MA, et al: Acupuncture for hot flashes: Decision making by breast cancer survivors. J Am Board Fam Med 25:323-332, 2012.
10. Crew KD, Capodice JL, Greenlee H, et al: Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol 28:1154-1160, 2010.
11. Garcia MK, McQuade J, Haddad R, et al: Systematic review of acupuncture in cancer care: A synthesis of the evidence. J Clin Oncol 31:952-960, 2013.
12. Schröder S, Liepert J, Remppis A, et al: Acupuncture treatment improves nerve conduction in peripheral neuropathy. Eur J Neurol 14:276-281, 2007.
13. Ahn AC, Bennani T, Freeman R, et al: Two styles of acupuncture for treating painful diabetic neuropathy—A pilot randomised control trial. Acupunct Med 25:11-17, 2007.
14. Phillips KD, Skelton WD, Hand GA: Effect of acupuncture administered in a group setting on pain and subjective peripheral neuropathy in persons with human immunodeficiency virus disease. J Altern Complement Med 10:449-455, 2004.
15. Shlay JC, Chaloner K, Max MB, et al: Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: A randomized controlled trial. Terry Beirn Community Programs for Clinical Research on AIDS. JAMA 280:1590-1595, 1998.
16. Bao T, Goloubeva O, Pelser C, et al: A pilot study of acupuncture in treating bortezomib-induced peripheral neuropathy in patients with multiple myeloma. Integr Cancer Ther 13:396-404, 2014.
17. Donald GK, Tobin I, Stringer J: Evaluation of acupuncture in the management of chemotherapy-induced peripheral neuropathy. Acupunct Med 29:230-233, 2011.
18. Xu WR, Hua BJ, Hou W, et al: [Clinical randomized controlled study on acupuncture for treatment of peripheral neuropathy induced by chemotherapeutic drugs]. Zhongguo Zhen Jiu 30:457-460, 2010.
19. Garcia MK, Cohen L, Guo Y, et al: Electroacupuncture for thalidomide/bortezomib-induced peripheral neuropathy in multiple myeloma: A feasibility study. J Hematol Oncol 7:41, 2014.
20. Han X, Wang L, Shi H, et al: Acupuncture combined with methylcobalamin for the treatment of chemotherapy-induced peripheral neuropathy in patients with multiple myeloma. BMC Cancer 17:40, 2017.
21. Greenlee H, Crew KD, Capodice J, et al: Randomized sham-controlled pilot trial of weekly electro-acupuncture for the prevention of taxane-induced peripheral neuropathy in women with early stage breast cancer. Breast Cancer Res Treat 156:453-464, 2016.
22. Rostock M, Jaroslawski K, Guethlin C, et al: Chemotherapy-induced peripheral neuropathy in cancer patients: A four-arm randomized trial on the effectiveness of electroacupuncture. Evid Based Complement Alternat Med 2013:349653, 2013.
23. Zijlstra FJ, van den Berg-de Lange I, Huygen FJ, et al: Anti-inflammatory actions of acupuncture. Mediators Inflamm 12:59-69, 2003.
24. Zhao ZQ: Neural mechanism underlying acupuncture analgesia. Prog Neurobiol 85:355-375, 2008.
25. Schroeder S, Meyer-Hamme G, Epplée S: Acupuncture for chemotherapy-induced peripheral neuropathy: A pilot study using neurography. Acupunct Med 30:4-7, 2012.
26. Chen ZX, Li Y, Zhang XG, et al: Sham electroacupuncture methods in randomized controlled trials. Sci Rep 7:40837, 2017.
27. Zia FZ, Olaku O, Bao T, et al: The National Cancer Institute’s Conference on Acupuncture for Symptom Management in Oncology: State of the Science, Evidence, and Research Gaps. J Natl Cancer Inst Monogr 2017(52), 2017.

